INTRODUCTION
All hypnosis is ultimately self-hypnosis, necessitating the patient's active participation in the process and experience. From the perspective of the practicing clinician, hypnosis is a useful way to help patients strategically refocus their presenting problems, their approaches to present-day living, and their stated goals. Clinicians from every therapeutic persuasion can teach patients self-hypnotic techniques to augment their own style of treatment; patients with many different diagnoses can benefit from the therapeutic gains afforded by the techniques.
Hypnosis is a process that can be useful in psychotherapeutic interaction, but it is neither a psychotherapy per se nor an independent medical or psychological art. It figured significantly in the development of psychotherapy, however, and its psychotherapeutic use often involves an intensification of the therapeutic relationship and of transference and countertransference. Although appreciation for the intensification of the dyadic relationship is necessary for the appropriate use of hypnosis in clinical practice, its application does not require adherence to a specific psychotherapeutic orientation. Hypnosis has been used by various proponents of most of the major psychotherapeutic paradigms -- from psychoanalysis to behavior therapy. In recent years its use has flourished partly as a result of an ever-increasing number of psychotherapies and eclectic treatment approaches that utilize adjunctive techniques, partly because of widening recognition of its clinical utility for certain disorders, and partly owing to advances in scientific understanding of the phenomenon.
What sets hypnosis apart from other adjunctive techniques and compels its consideration as a psychotherapeutic process is that it typically involves significant changes in the dyadic relationship of patient and therapist. It is the interpersonal alteration in the midst of an ongoing psychotherapeutic relationship that characterizes hypnosis and requires an understanding of the undercurrents and processes that it engenders. If those issues are not understood, the therapeutic gains that can be obtained with hypnosis can result in the false impression that a clinician can use hypnosis to treat patients whom the therapist is not otherwise qualified or experienced enough to treat without hypnosis. Although it can provide therapeutic advantages, hypnosis should never be used to treat a condition that the therapist is unprepared to treat without it.
PHENOMENA OF HYPNOSIS Controversy over the nature of hypnosis and its utility as a construct has existed since the phenomenon was first described. It has been variously theorized to be an altered state of consciousness, a dissociated state, an access to the unconscious, a form of conditioning, and a compliant response to suggestion or social cues. The professional literature teems with metaphors and descriptive phrases intended to capture its theoretical essence, including the concepts of fantasy absorption, believed-in imaginings, role enactment, focused attention, loss of generalized reality orientation, goal-directed fantasy, regression in the service of the ego, archaic involvement, and altered brain function. However, such hypothetical constructs have proved to be extremely difficult to operationalize empirically.
The problem is partly a result of the fact that hypnosis has no known unique psychophysiology or neurobehavioral basis and thus cannot be distinguished as, for example, sleep can from wakefulness. By and large, the hypnotized subject appears to be in a state of relaxed wakefulness, but not sleep. Sleep onset and sleep stages are easily distinguished from wakefulness and hypnosis by specific changes in the electroencephalogram (EEG) and other psychophysiological parameters. However, using only psychophysiological measures, hypnosis cannot, as yet, be reliably discriminated from other nonsleep states or conditions. That fact does not mean that hypnosis lacks uniqueness. Even though there is no neurophysiological measure for distinguishing among other waking states in general (whether or not they are conceptualized as altered), including those states characterized by intense differences (for example, emotional states), no one disputes their experiential validity or the profound differences in behavior that they produce.
Rather than attempting to define hypnosis in terms of abstract hypothetical constructs or neurophysiological conjecture, it is useful to discuss what essentially everyone who has ever worked with hypnosis agrees are the phenomena that it can evoke -- specifically, the phenomena that occur rarely or only under very special circumstances outside of hypnosis. Those phenomena need to be distinguished from the events that often accompany hypnosis but that do not require hypnosis in order to occur.
Distinguishing hypnosis from contextual demands Hypnosis is often portrayed as a technique whereby the hypnotist gains control over the subject in order to elicit behaviors that the subject would not otherwise exhibit. A stage hypnotist, for example, might suggest to volunteers that they are chickens and get them to behave as chickens in front of an audience. The apparent ability to induce otherwise normal persons to engage in embarrassing acts in public seems as awesome as it is amusing, and thus there is a strong tendency to attribute the power of hypnosis to the hypnotist, with little regard for the expectations inherent in the context in which the hypnosis is carried out.
Because of the still common popular misconception about the power of the hypnotist, it is the first author's practice to begin a lecture on hypnosis for medical students by asking one of the students for a left shoe, another for a wallet, a third for a watch, and a fourth to exchange eyeglasses with a fifth student. Over many years of doing this classroom experiment, only once has a student refused to comply with those requests. When the persons who cooperate are asked whether they were hypnotized, they correctly answer that they were not. When asked why they carried out the actions, they respond, "Because you as the profes-
1807
1808 PSYCHOTHERAPIES/CHAPTER 31
sor requested it, and it was a class demonstration." If the students had been hypnotized before the demonstration, observers would tend to attribute their behavior to the power of hypnosis, whereas the behavioral control was actually a function of the student-teacher relationship, which is not normally exploited in that fashion.
In a similar way demonstrations have been conducted in an experimental context that show unhypnotized subjects willing to engage in ostensibly dangerous acts. Although they were not informed that the conditions were structured to prevent anyone from being hurt, most subjects in an experiment were willing, upon being asked, to extract a penny from fuming nitric acid, pick up a poisonous snake, or throw acid at a research assistant. In the past investigators attributed the elicitation of such behaviors to the hypnosis instead of to the demands inherent in the experimental context and to the fact that subjects knew that the experimenter was responsible for their safety and that care must have been taken to ensure that no one would be injured.
The demonstration that unhypnotized persons will carry out such acts in various contexts illustrates a crucial point: it is necessary to determine what a motivated person is willing to do in a particular context without hypnosis before assuming that actions observed in hypnosis are uniquely a function of the hypnosis. It is not known whether hypnosis can increase compliance beyond that attributable to the demands of the situation. However, it is clear that compliance, as such, does not allow an observer to decide whether the subject was or was not hypnotized.
The confusion between what a person will do in hypnosis and what the person will do as a function of contextual demand characteristics has led to two extreme positions regarding the nature of hypnosis. In one view, all hypnotic and much nonhypnotic behavior is attributed to the hypnotic state, which is often then argued to be a product of a person’s ability to slip in and out of hypnosis at any time; as a result any behavior at any time can be attributed to hypnosis. The other view holds that demand characteristics account for all hypnotic behavior, and that there is, therefore, no state of hypnosis, but only varying degrees of compliance in hypnotic contexts. Attributing either everything or nothing to hypnosis makes it difficult to study systematically those features that largely characterize hypnosis.
Domain of hypnosis The phenomena that characterize hypnosis typically involve changes in the hypnotized person's subjective experience, changes that the person cannot readily bring about without hypnosis. For example, if unhypnotized subjects are asked to forget the word "hippopotamus," they typically are unable to do so, and the harder they try, the less likely it is that they will succeed. Similarly, someone in pain is rarely able to stop the pain at will. If asked to see someone who is not there, a subject may be able to visualize the person but does not confuse the visual image with an actual person.
Hypnosis, however, can facilitate the ability to forget the word "hippopotamus," to block the appreciation of pain, and to confuse an imaginary image with an actual person. Thus, careful consideration of those subjective changes that can be brought about by hypnosis, and that the subject actually identifies as what is experienced, indicates that hypnosis is best characterized by alterations of memory, perception, and mood in response to suggestion, rather than by overt behavioral changes.
In general, hypnotic experience and behavior are correlated in such a way that behavior can be used to estimate the degree of experiential change, although there are many events that can occur during hypnosis that do not permit the determination of whether or not they are related to the hypnosis. Still, if a person who experiences pain during a medical procedure is hypnotized and then does not report pain, it is reasonable to consider the behavioral report as reflecting an alteration of perception brought about by hypnosis.
Whether someone is hypnotized, and if so, the extent to which the hypnosis is experienced, involves a diagnostic assessment that should be predicated on the person's response to hypnotic suggestions. The extent to which a person is able to respond to suggestions that involve alterations of perception, memory, or mood, and the degree to which these alterations are subjectively compelling to the subject are the basis for deciding whether hypnosis has taken place. Like all diagnostic procedures, it depends on the diagnostician’s skill and the subject's willingness to describe experiences honestly.
It is important in a clinical context to explore the subjective experiences of a patient who has been exposed to a hypnotic induction procedure, because behavioral response to suggestion can sometimes be misleading. For example, if during the induction of hypnosis it is suggested that a subject's right hand is growing lighter because the fingers are attached to helium-filled balloons that are floating upward, then there is likely to be a close relationship between the extent to which the hand moves upward and the likelihood that the subject will be able to experience other aspects of hypnosis. The reason for the relationship is that the subject is not told to raise the hand, but rather to imagine that the hand is light, which involves an alteration of perception. To the extent that the subject perceives the hand as light, there is likely to be some overt movement of the hand: it is also true that the person may feel considerable lightness in the hand with little upward movement. In either case it is the subjective description of the perception that is important in determining the extent to which the suggestion induced an altered perception.
DEFINITION Hypnosis is that state or condition in which a person is able to respond to appropriate suggestions by experiencing alterations of perception, memory, or mood. The essential feature of the phenomenon is the subjective experiential change. Overt behavior is useful to index the change, but it must be assessed in the particular context by a suitable inquiry into the experience of the patient. From the point of view of an outside observer, hypnosis is characterized by the hypnotized subject's increased suggestibility and suspension of critical judgment.
EVOLUTION OF HYPNOSIS Precisely how a hypnotized person behaves is a function of the beliefs and expectations that the subject and the hypnotist share about hypnosis. Those beliefs and expectations are in large part culturally determined, which is, perhaps, the most important lesson to be learned from the historical evolution of hypnosis.
Hypnosis or hypnoticlike processes have long been a common feature of various religious, ceremonial, and healing practices. However, the precise behavioral characteristics seen when persons are hypnotized vary among cultures and over time. Hypnotic techniques date back to antiquity, as in the healing practices of ancient Egypt and Greece. The Egyptians described hypnoticlike procedures in the "Ebers Papyrus," and sleep healing at the Temple of Asclepius in ancient Greece has been conceptualized as analogous to hypnosis. Trancelike behavior attributed to spirit or divine possession has played a role in the mystic traditions of Judaism, Islam, Christianity, and mans other religions. Powers ascribed to shamans and the art of faith healing are probably related to hypnosis.
Mesmerism Modern hypnosis is usually traced to the Austrian physician Franz Anton Mesmer (1734-1815), who worked in France during the time of the American Revolution. He originally studied the effects of celestial bodies on human lives, but then became interested in the effects of magnetism. Mesmer observed that exposure to magnets could have profound healing effects. Later, he realized that magnets were not crucial for these therapeutic effects; it often was sufficient for him to touch the person or the water contained in large wooden tubs with an iron rod. Mesmer thus recognized that the power was not in the magnet but in himself; the result was the concept of animal magnetism, which he thought of as a fluid that he could store and transfer to others. As an example, a follower of Mesmer, Marquis Chastenet de Puysegur, "magnetized" a tree on his estate from which his peasants could obtain relief for their ailments. The marquis then discovered that merely talking to a person could influence the ailment. He tried unsuccessfully to get Mesmer to study the power of suggestion, but Mesmer preferred to investigate what he considered to be the physical causes of cure.
Given present knowledge, it is easy to see that Mesmer's reasoning was not logical when he concluded that if the curative power did not reside in the magnet, then a magnetic force in the magnetizer must have effected the cure. However, Mesmer was a physician and a product of the age of reason, and offering physical causes for what appeared to be physical events was the only scientific view that was generally acceptable to his profession at that time. The age of psychology was not to dawn until 100 years later. At the time of Mesmer, the concept of physical conditions, as opposed to mental or psychosomatic conditions, was not well elaborated. The differentiation between hysterical illness and organic lesion was yet to be made. Thus, Mesmer did not appreciate that the treatments were not physiological but psychological in nature, and were primarily effective for what later would be called functional, hysterical, neurotic, or psychosomatic disorders.
Some of Mesmer's healing procedures were in ways analogous to current hypnotic practices. The sessions typically included a variety of implicit suggestions given to patients in a setting that facilitated relaxation, a belief in the magnetizer's abilities, and expectations that dramatic events were to take place. The behavior expected of the mesmerized patient was also communicated in those sessions. There was a strong element of social contagion as the course of magnetic treatment culminated in a mesmeric crisis, which appeared to be a hysterical fit. Patients awoke from the crisis with varying degrees of symptomatic relief. The use of the term "crisis" was probably associated with an
1809 HYPNOSIS
18th-century view that many illnesses (for example, most febrile illnesses) followed a course that ended in crisis, which if the person survived, was followed by dramatic improvement. It seems likely that the hysterical seizures seen in the mesmeric crisis were modeled after epileptic seizures that were already well known.
In that sense animal magnetism provided a metaphor for the healing powers of faith, belief, and a meaningful interpersonal relationship. Although Mesmer 's theory of cure was incorrect, he effectively demonstrated the healing power inherent in the therapeutic relationship. Unfortunately, he also polarized the attitudes toward his work in ways that have persisted to the present day.
Because of the controversy surrounding mesmerism and the notoriety that followed Mesmer's therapeutic claims, as well as the behavior of the man himself, a commission was convened to investigate the procedure. Headed by the American diplomat and scientist Benjamin Franklin, it included the French chemist Antoine-Laurent Lavoisier and physician Jacques Guillotin. The group devised a number of experimental procedures that failed to document the existence of animal magnetism and showed that the subject's beliefs, rather than the specific behaviors of the magnetizer, were responsible for the consequences of mesmerism. In its report the commission acknowledged the dramatic relief often obtained by patients of the magnetizer, but dismissed the mechanism as nothing more than imagination. That conclusion had the effect of associating mesmerism with quackery, because the role of imagination in curing certain illnesses did not appear to be worthy of further consideration. Mesmer's claim of the existence of an invisible fluid -- animal magnetism -- was false, but the conclusion that the therapeutic effects of the technique vis-à-vis imagination were not worth considering was equally false.
There is another aspect of Mesmer's work that has turned out to be a precursor of basic therapeutic insights. In addition to the commission's report, there was a secret report to the king of France, which explained that because many female patients developed strong erotic feelings toward the magnetizer, the technique constituted a serious threat to public morality. That report anticipated the concept of transference and its potential complications.
Hypnotism The next milestone in the evolution of hypnoticlike therapy procedures was marked by the work of the Scottish surgeon James Braid, who coined the term "hypnosis" (from the Greek word for sleep) in the 1840s. Having observed magnetic therapy, Braid felt that the crucial factor in mesmeric treatment was the focusing of attention (monoideism), and that the process would lead to an artificial somnambulism, which he called hypnotism. Thus, Braid shifted the metaphor from the mesmeric crisis to one of artificial sleep, during which a person responds to suggestions. Eye closure, relaxation, and the apparent automatic response to suggestions became the hallmarks of the phenomenon. Braid, and those who followed him, no longer observed the hysterical seizures that the magnetizers had induced. However, the curative effects of Braid's hypnotism were very similar to those of Mesmer.
By the late 19th century interest in hypnosis increased as a result of another major controversy in France. The French neurologist Jean-Martin Charcot, who helped delineate hysterical paralyses from paralyses related to neurological deficits, also studied the effect of metals on disease and eventually became interested in hypnotism. He believed that hypnosis resulted from a physical process and constituted a physiological state that followed a clearly delineated course; for example, rubbing the top of a subject's head was thought to shift the patient from seep to somnambulism. Charcot demonstrated hypnotic effects with his patients, believing that it was a pathological state that occurred in those who suffered from hysteria. His interest in hypnosis lent an air of respectability to the phenomenon, because he described it in neurophysiological terms.
A professor of medicine and contemporary of Charcot, Hippolite Bernheim, maintained that hypnosis involved neither physical forces nor physiological processes, but rather was a psychologically mediated response to suggestions. Bernheim also used hypnosis extensively with his patients, arguing that it was not pathological and that there was no hypnosis but rather only suggestion. He demonstrated that hypnotic phenomena could be elicited without inducing the sleeplike condition that characterized the work of Braid and Charcot and their students. In his book Suggestive Therapeutics, Bernheim stated that the fact that he could induce the classic phenomena of hypnosis in suitable persons without a formal hypnotic induction procedure challenged the physical (sleep-related) theories proposed by Charcot and others.
Hypnotic behavior Although it is controversial as to whether there are specific physiological markers for hypnosis (none have so far been documented), the verdict of history indicates that Bemheim's view of hypnosis was considerably closer to the mark than was that of Charcot. Bernheim was correct in that no unique behavioral course of events characterizes hypnosis. Thus, the mesmeric crisis, Braid's artificial sleep, and the carefully delineated hypnotic stages of Charcot have all proved to be related to the expectations of the subject and the hypnotist, which, in turn, came from the cultural matrix at the time each of those persons lived.
The first author carried out an experiment to test the role that expectation and belief play in shaping hypnotic behavior. Two large classes of students were given a lecture, including a demonstration, on hypnosis. Unbeknownst to either class, three highly hypnotizable subjects were given a suggestion prior to the demonstration that during the demonstration they would experience catalepsy of the dominant hand (unilateral catalepsy has never been described in the literature as an event that naturally characterizes hypnosis). The only difference between the two classes was that catalepsy was tested only in one class, where it was casually pointed out during the demonstration that catalepsy of the dominant hand is typical of deep hypnosis. Three weeks later students randomly selected from both classes were hypnotized. Several from the class exposed to the unilateral catalepsy demonstration developed it spontaneously during hypnosis, thereby confirming that expectations and beliefs about hypnosis influence the behavioral manifestations of the phenomenon.
That simple experiment seems to provide an empirical demonstration of why and how the behavioral characteristics of hypnosis could have changed so easily, depending on the beliefs of both the hypnotist and the subject. It supports the view that behavioral characteristics are not adequate to identify the hypnotic phenomenon, and it underscores the fact that any set of behaviors that subjects believe to be characteristic of hypnosis can be manifest in their hypnotic behavior. Thus, the behavioral differences seen among mesmeric crisis, Braid's artificial sleep, and the hypnotic stages of Charcot probably reflected the expectations and beliefs about the phenomenon present at those various times. Such expectations and beliefs of both the hypnotist and the subject can also influence the content of recovered memories.
Dynamic psychotherapy The practice of mesmerism and hypnotism through the mid-19th century involved the use of direct hypnotic suggestion to ameliorate specific symptoms. When Sigmund Freud returned from France, where he had been greatly impressed by the therapeutic potential of hypnosis for neurotic disorders, a collaboration was begun with Josef Breuer to develop a radically new approach to treatment with hypnosis. Rather than using hypnosis to suggest that a symptom would cease to be a problem, they used it to help the patient remember traumatic life events that appeared to be at the root of the current symptom. Freud observed that his patients would often appear to relive the traumatic events in hypnosis, abreacting with intense affect and describing events that apparently could only be known if the patient had actually been there. On awakening from hypnosis patients would seem to obtain relief from the particular symptom involved. As Freud began to develop psychoanalysis, theoretical considerations, as well as the difficulty he encountered in hypnotizing some patients, led him to discard hypnosis in favor of free association. Although Freud rejected hypnosis as part of psychoanalysis, he continued to view it as an important technique in the study of unconscious phenomena. Hypnosis as an uncovering technique has continued as an accepted adjunct to dynamic psychiatry.
Though eclipsed by the preeminence of the psychoanalytic school, the French psychiatrist Pierre Janet and American psychiatrists, including Morton Prince and Boris Sidis, continued to use hypnosis in a different conceptual framework. They focused on the concept of dissociation, which was common to certain neurotic disorders and occurred during hypnosis. Both World War I and World War II led to a resurgence of interest in hypnosis as a means to treat what was called shell shock in World War I, combat neuroses in World War II, and more recently, posttraumatic stress disorder. The modern era of hypnosis research began after World War II, with a surge of systematic studies; a reevaluation of earlier concepts, such as dissociation; and the development of better techniques for assessing hypnotic responsivity.
ELEMENTS OF HYPNOSIS
HYPNOTIZABILITY The ability to experience suggested distortions varies considerably among people, but it is not the same as compliance, conformity, gullibility, or persuasibility. Some persons are highly responsive to suggestions for altering their subjective experience; others are not. That responsiveness dimension, called hypnotizability, remains a remarkably stable attribute of a person throughout adult life. Hypnotizability is evaluated clinically by the person's responsiveness to suggestions following induction, and may be measured systematically by standardized tests.
The recognition of the importance of hypnotizability was a major development because it refocused attention away from
1810 PSYCHOTHERAPIES / CHAPTER 31
the power or skill of the hypnotist and directed it toward the patient's capacity to respond to suggestions. Since Bernheim first described a scale of hypnotic responsivity more than 100 years ago, a number of scales have been developed to assess responsivity to hypnotic suggestion. Those scales characteristically contain four classes of suggestion: ideomotor items, challenge items, cognitive items, and memory items.
Ideomotor items involve suggested changes in motor experiences and physical movements. The sway test, in which it is suggested that a subject think about falling backward, is a typical example of that class of suggestion. If the sway test is given in the appropriate hypnotic context, the responsive subject will feel like falling backward, and may actually do so. In a medical setting a common ideomotor item involves the suggestion that the arm is growing lighter and that it will float upward like a balloon. Ideomotor suggestions are often the easiest to experience.
Challenge items involve a suggested inability to carry out an action. For example, it may be suggested that the arm of a hypnotized person is straight and rigid, like a bar of steel, and that the person will be unable to bend it. If the subject is unable to bend the arm, even after encouragement to do so, it is considered that the challenge suggestion has been experienced. A wide variety of challenge suggestions have been used (for example, the suggestion that the subject's eyes cannot be opened). As compared with ideomotor suggestions, challenge suggestions are experienced by fewer subjects and are considered more difficult. They are generally avoided in clinical work with hypnosis because they may foster a power struggle between the patient and therapist.
The third category of suggestions involves cognitive alterations or suggested hallucinations. An example is a suggestion that the person imagine himself or herself on a beach, relaxing in the warmth of the sun, taking in the sight, sound, and smell of the surf (that is, positive hallucinations). Similarly, it can be suggested that a patient will not perceive a stimulus, as in the case of pain, or will hear only the voice of the hypnotist (that is, negative hallucinations). Such cognitive suggestions can vary in difficulty, but are often the most important suggestions used in therapy.
Finally, important hypnotic suggestions associated with changes in memory deserve special mention, given their history in the clinical use of hypnosis. Examples would be suggestions that a person be unable to remember what has occurred during hypnosis (that is, posthypnotic amnesia), or more relevant therapeutically, that a person will be able to recall, and perhaps relive, events of the past that may appear to be unavailable to consciousness (that is, hypnotic age regression and hypnotic hypermnesia). The use of hypnosis to block or unblock memory processes has a long and controversial tradition and continues to be a common feature of the clinical application of hypnosis but requires caution as described below.
In recent years much psychometric work has been done on the development of reliable and stable scales of hypnotic responsivity, which typically include all four classes of items. Standardized scales are necessary because the same suggestion can vary in difficulty, depending on the manner in which it is administered. Thus, the Stanford Scales of Hypnotic Susceptibility, which use 12 items, are more stable and useful for scientific work because the administration of each item to subjects is carefully standardized. It is critical, however, that the clinician understand what constitutes a difficult versus an easy suggestion for a given patient, in order to assess how a patient is responding and thus avoid the patient's experiencing unnecessary failure. An advantage of the hypnotic susceptibility scale is the so-called item-pass percent, which can be assessed for any given item to determine its difficulty.
INDUCTION Most of what has been written about how hypnosis is most effectively brought about focuses on the induction techniques. It should be clear that hypnosis is a function of the subject's ability rather than the hypnotist's skill, and, therefore, the induction of hypnosis in a cooperative subject requires little special expertise. Most tests of hypnotizability involve verbatim presentation of hypnotic induction spiels. Although there are innumerable techniques for inducing hypnosis, and some may seem more effective than others in certain patients, induction is best understood as a broader process that includes the preconditions that facilitate the therapeutic use of hypnosis.
Rapport Induction procedures typically begin with the comment, "First one establishes rapport," and continue with a description of what the authors view as the important (technical) aspect of the induction procedure. It is the establishment of rapport, however, that is the most important component of an induction procedure. Thus, it is necessary to have the. kind of relationship that justifies the induction of hypnosis as appropriate by both the patient and the clinician. It is helpful for the patient to understand the reason why hypnosis is to be used and to recognize the necessity for his or her active participation. Any concerns the patient might have about what may happen during hypnosis (for example, its effects, whether the patient will be able to maintain control, or whether the patient will be different in any regard in the future) should be clarified. Because hypnosis is carried out in an interpersonal relationship in which both parties need to participate actively, it is not appropriate to speak of doing hypnosis to someone, but rather of doing hypnosis with a properly informed cooperative patient.
Before a person is hypnotized, the therapist should understand what the patient hopes to gain by hypnosis, including the overt expectations, as well as any hidden agenda, that the patient might have brought to the clinical context. Ultimately, the establishment of rapport must include clarifying for the patient that hypnosis is a therapeutically acceptable procedure. that may be of some benefit to the patient, that the patient can experience it at some level and use it to some extent to cope, and that the therapist is a competent person who will help the patient use hypnosis.
Although most persons have the capacity to be hypnotized, albeit in varying degrees, it is relatively easy to prevent a person from responding to it. For example, if the subject feels that responding to hypnosis is inappropriate, or if a power struggle is set up between the therapist and the subject, even highly responsive persons will fail to respond. Thus, the patient who believes that only gullible or weak-willed persons can be hypnotized is likely to resist hypnosis. Similarly, a patient who has seen a stage performance in which hypnotized volunteers were used as objects of fun and ridicule may appear unresponsive to hypnosis if the differences from its medical use are not discussed. Again, a lack of response would not be the result of an innate lack of ability, but the product of a negative view toward being hypnotized.
Establishing rapport with a patient thus should include an inquiry into the person's beliefs about and experiences with hypnosis. For example, if the patient has a negative attitude toward hypnosis as a result of watching a hypnotist perform on stage, it should be explained that volunteers from the audience are aware that it is for entertainment purposes, and they are willing to become the object of fun in exchange for being the center of attention, whereas the purpose of hypnosis in the therapeutic context is to treat the patient and not to entertain someone else. If a patient knows someone who has had an unfortunate experience with a lay hypnotist, it is helpful to explain that the induction of hypnosis is relatively easy with a cooperative subject, but that a physician or psychologist who utilizes hypnosis in treatment is trained to know when and how to use it.
The appropriate development of rapport in order to use hypnosis involves addressing a patient's real concerns and interests; it cannot be achieved by lecturing to a patient. The most effective approach is to encourage questions from the patient. Such questions should not be considered as difficulties created by the patient that are to be disposed of as quickly as possible, but as an opportunity to communicate in a context in which the patient attends to what is being said. When a patient asks a question, no matter how anxious, angry, or upset the person may be, there is an expectation that the therapist will answer it. Consequently, questions by a patient are an opportunity to make clear those points that the therapist wishes to communicate regarding hypnosis.
If the therapist brings up the possibility of using hypnosis, a patient may inquire, "Do you really hypnotize people?" The way the question should be answered depends on the therapist's perception of what is really being asked. For example, if the patient seems to be very con-
1811 HYPNOSIS
cerned about autonomy, it may be helpful to say, "It is the patient who chooses to go into hypnosis, and all anyone can do to help this process is to guide the way, because all hypnosis is really self-hypnosis." The same message may be amplified by pointing out, "If someone wants to enter hypnosis, it is generally easy to do so because it is really all self-hypnosis. I have found that the vast majority of patients who want to use the hypnotic mode have no trouble responding to it." Here, the idea implicitly added is that most people can respond without difficulty. Or the therapist could say, "Most people who have good powers of concentration are able to respond." The point is that, in the context of answering a question, it is easy to communicate important attitudes and information that would not otherwise be readily accepted.
The purpose of rapport building is to enhance the therapeutic alliance by having the patient feel comfortable with the idea of hypnosis, anticipate that there will be no problem experiencing it, and understand that the therapist can help in its use. With those goals in mind, the therapist should solicit and answer questions in a way that also communicates what will help the patient respond appropriately.
It is crucial that the therapist who uses hypnosis recognize that the ability to respond is inherent in the patient, and that the task of inducing hypnosis depends on that inherent ability. However, for hypnosis to take place, it is important to create the kind of rapport in which the patient feels comfortable and safe, and perceives the therapist as someone who is capable of helping the patient. The preconditions of the relationship between the therapist and patient for the induction of hypnosis are similar to the preconditions that make for successful psychotherapy.
Therapist attitudes One important phenomenon that is accentuated when hypnosis is used is the tendency to perceive the therapeutic relationship as a power struggle in which either the patient or the therapist views the hypnosis as somehow controlling the patient.
Among the many reasons why Freud chose to abandon hypnosis in his therapeutic approach was his view that it was not useful because not everyone could be hypnotized. That fact, however, should not prevent the therapeutic use of hypnosis for those persons who can be hypnotized, just as physicians do not reject treatment with a particular drug because it is effective for only some of their patients.
Unfortunately, many therapists who use hypnosis view its induction in a patient as an achievement. If the therapist takes credit for the induction of hypnosis, however, it then becomes a narcissistic injury when a patient fails to enter hypnosis, because the therapist feels compelled to take responsibility for the failure. Even today many therapists working with hypnosis say it is not useful for some patients because they were unable to hypnotize those patients. Yet the same therapists, when meeting a patient who has little verbal facility and is unable to discuss problems, will say that the patient does not have the ability to talk about problems and so dynamically oriented psychotherapy is unsuitable for that patient -- in other words, it is the patient's problem.
As with any psychotherapeutic endeavor, the correct formulation with regard to hypnosis is the statement that the patient does not have the ability or the motivation to respond. The therapist can only provide the context that will minimize those factors that prevent hypnosis in a patient who can respond. For the optimal use of hypnosis in treatment, it is essential that the therapist not be unduly concerned with hypnotizing every patient but understand the necessity to make clear to the patient that it is the patient who seeks help and it is the patient who would benefit from hypnosis.
Hypnosis is often most effective for a therapist after the therapist has become bored by its induction and has transcended the power fantasy engendered by the initial observation of a patient entering hypnosis. Power fantasies and struggles, even if they do not prevent the patient from entering hypnosis, will have deleterious consequences in the therapeutic context and should be avoided. Some induction procedures, such as using the therapist's eyes as fixation points for the patient's eyes, are undesirable because they encourage confrontational fantasy. Instead, techniques that are low key, that emphasize the patient's contribution and desire to enter hypnosis, should be utilized. One of the values of learning to use hypnosis as an adjunct to psychotherapy is the increased awareness by the therapist of subtle nonverbal exchanges that affect the processes inherent in all forms of psychotherapy.
Maximizing patient response Although the establishment of rapport by dealing with a patient's concerns about hypnosis is a major factor in creating an appropriate setting to optimize its therapeutic effects, there are a number of specific procedures to help the patient realize that the therapist can help to bring about the experience of hypnosis.
Those procedures involve capitalizing on some naturally occurring hypnosislike phenomena that are ubiquitous and are likely to have occurred in the lives of most patients. For example, when discussing what hypnosis is like with a patient, the therapist may ask, "Have you ever been preoccupied with thinking about some issue while driving home and suddenly realize that, although you have arrived safe and sound, you cannot recall having driven past familiar landmarks? You stopped at all the red lights and you avoided collisions. You were somehow traveling on automatic pilot." Most persons resonate to this experience and will describe similar personal experiences. Such discussions make clear that patients have the capacity to utilize the hypnotic mode, as it is merely an extension of those kinds of experiences. Although such experiences do not necessarily involve hypnosis, the extent to which a person experiences them is correlated with hypnotizability.
Another way to maximize a patient's response to hypnosis in the clinical context is to have the patient participate in a brief demonstration of a procedure that promotes better understanding of what hypnosis might be like. Two such procedures are the Kohnstamm phenomenon and the Chevreul pendulum. Both are subjectively compelling, virtually everyone can carry them out, and, if done properly, they help to convince patients that they can respond to hypnosis.
KOHNSTAMM PHENOMENON The Kohnstamm phenomenon involves mildly fatiguing a muscle in the arm by pushing both arms against a doorjamb and then, after stepping away, experiencing the arm as feeling light and floating upward. Before demonstrating the phenomenon in a patient, it is best to point out that it is not a hypnotic event, but a natural physiological response of the body. However, it can help the patient learn about responding without volitional effort.
In that sense the Kohnstamm phenomenon serves as an estimate of the patient's readiness for hypnosis. Although it is a physiological response, the Kohnstamm phenomenon is easily prevented by a patient, and in that regard is similar to hypnosis. It generally affords the patient a feeling of mastery, as well as the recognition that hypnosis will require active cooperation and can easily be blocked if the patient chooses to do so.
CHEVREUL PENDULUM The phenomenon of the Chevreul pendulum is a classic ideomotor effect. A ring, a key, or some other small object tied to a string can serve as the pendulum; the string is usually about 30 cm in length. (It is desirable to use a common object rather than a crystal ball or a watch on a chain, which are too reminiscent of stage props.)
Before demonstrating the effect, it should be explained to the patient that when a person thinks intensely about an idea involving a particular motor action, there is a tendency to make minute movements consistent with the action. For example, someone who is engrossed in watching a boxing match will often show small movements that mimic the blow-by-blow action. The therapist can then demonstrate the phenomenon to the patient by holding the string end that is not attached to the weight (for example, a ring), thereby suspending the weight in the air, with the elbow of the arm (holding the string) resting on a desk top or the arm of a chair. It should be pointed out to the patient that as the therapist thinks about the weight moving backward and forward, the weight will begin to move. Typically, the movement response takes a few moments to develop. When excursion reaches approximately 10 cm, the therapist may change the direction of the weight by thinking about a circular motion. That change (in thought) should be explained to the patient. The ring then will begin to move in an elliptical pattern, and soon thereafter in a circular path. At that point the therapist indicates that to stop the ring by thinking about it is the most difficult aspect of the exercise. As the therapist focuses on that maneuver, the ring will make smaller and smaller excursions, and eventually will come to an almost steady position.
On completing the demonstration, the therapist should ask the patient to try it, making clear that the patient should avoid consciously moving the pendulum. Although many patients are initially skeptical, they are soon amazed to find that as they concentrate on the weight and think about the motion of swinging backward and forward, the weight actually reflects their thought and begins to move. Occasionally, a patient may move the hand holding the string, at which time it is important for the therapist to point out that it should happen nonvolitionally.
As with the Kohnstamm phenomenon, the ideomotor effect seen in the Chevreul pendulum demonstration is related to readiness for hypnosis, and even patients with very little hypnotic capacity will be able to experience compelling ideomotor responses with the pendulum. A successful experience with the pendulum will maximize the likelihood of a hypnotic response. Likewise, if a person fails to respond to the pendulum, it may be best not to continue to hypnotic procedures, even if the patient asserts a readiness to do so, until the patient no longer blocks the usual ideomotor response.
Both the Kohnstamm phenomenon and the Chevreul pendulum are useful in helping patients appreciate that they can respond to ideas, which, in turn, facilitates responsiveness to hypnosis. The procedures also can serve to alert the therapist to those patients who are likely to block their hypnotic responses unless hypnosis is discussed further with them.
SELF-HYPNOSIS
Most therapists who use hypnosis in treatment find it easy and effective to teach their patients self-hypnosis, which can be
1812 PSYCHOTHERAPIES / CHAPTER 31
practiced outside of the therapist's office. Virtually all hypnotic phenomena that can be suggested by the therapist can also be induced by the patient using self-hypnosis. For example, in the use of hypnosis for the treatment of pain, a therapist may suggest that the pain will collect in the fist as the patient focuses on the closing fist. Once the fist has closed, the therapist may suggest that the patient open the fist, discard the pain, and feel comfortable and relaxed. Like many hypnotic suggestions, the metaphor of gathering the pain and throwing it away need not be logical; to be helpful, it need only stimulate a fantasy that the patient can accept and from which the patient can benefit. After learning how to gather the pain and discard some or all of it, the person can be taught to carry out the exercise outside the therapist's office, by following a simple self-hypnosis procedure that reinforces the suggestion and maintains the patient's ability to experience little or no discomfort. Patients also can be taught to control phobic symptoms and symptoms of stress-related physiological response affecting medical conditions, as well as to reinforce the intention to control undesirable habits.
Although self-hypnosis may contain the essence of hypnosis, the likelihood of a patient's continuing to use self-hypnosis in a therapeutically helpful way appears to be enhanced by maintaining a relationship with a therapist. Despite the availability of many books on self-hypnosis, very few persons learn and continue to practice it without a teacher or therapist. Similarly, hypnosis audiotapes often do not continue to be effective without an interpersonal therapeutic relationship.
As a result of the apparent need to maintain such a relationship to enhance its effects, many clinicians ask patients who are using self-hypnosis to return for short sessions to reinforce the procedure. The frequency of the visits depends on the patient's ability to use self-hypnosis for the targeted symptoms. In some instances it is necessary to see a patient only occasionally, or to have a patient periodically send notes about progress. Even in those cases, however, it is important for a patient to maintain a positive relationship with the therapist and to feel that the therapist is available, if needed.
Although there may be reasons for wanting to terminate treatment formally, it may not be wise to do so if a patient continues to need to use self-hypnosis. Rather, the therapist should seek to titrate the relationship to maintain a patient's ability to use self-hypnosis with the least amount of time on the part of the therapist and the least cost on the part of the patient.
A self-hypnosis technique that is widely used in Europe and Asia is autogenic training. Taught individually or in groups, it consists of a series of systematic exercises (that is, self-suggestions of bodily changes) that the patient learns in a fixed sequence. The procedure was developed by Johannes Schultz to invoke the effects of meditative disciplines without mystic overtones. It has been taught in some European secondary schools as a prophylactic form of mental hygiene, and has been used successfully in the treatment of a wide range of psychosomatic difficulties. Schultz emphasized the ease with which a patient adept at autogenic training can enter a more traditional form of hypnosis. Many meditative disciplines and relaxation training procedures (such as Jacobson's Progressive Relaxation Technique), as well as some forms of biofeedback (notably muscle activity and skin temperature feedback), also involve processes similar to those found in hypnosis and self-hypnosis.
HYPNOSIS IN PSYCHOTHERAPY
Hypnosis is a technique, not a psychotherapy. For that reason different aspects of hypnosis are useful in different therapeutic approaches. As a technique, hypnosis should be integrated into the psychotherapeutic approach rather than used as something outside of the usual psychotherapeutic interaction. Unfortunately, many clinicians find it difficult to utilize hypnosis in the therapeutic context because of uncertainty about how it might change their approach to psychotherapy. Moreover, therapists who do become interested in its use will often change the relationship with a patient when applying it, as if the principles of treatment are obviated when hypnosis is induced.
The use of hypnosis does introduce different and novel expectancies on the part of a patient, but it should not do so for a therapist. The therapist must understand the consequences of a patient's expectations about hypnosis, as well as the hypnotic phenomenon itself when used in the context of psychotherapy. Perhaps the greatest problem is the need for a therapist to have had sufficient experience with hypnosis before using it in therapy. Preferably, the experience should be with healthy persons, where the question of psychopathology is irrelevant, in order to gain an appreciation of the role that a subject's ability to enter hypnosis has in bringing about the phenomenon. Although the behavior of a therapist may block a subject's response to hypnosis, it should be recognized that subjects' motivations and innate abilities to respond account for most of the variance among persons in response to an induction procedure. A therapist should be sufficiently familiar with the hypnotic response of normal persons in order to be neither surprised nor unduly gratified when a patient becomes hypnotized.
When a clinician first begins to work with hypnosis, there may be concern that a given patient may lack the ability to respond. That concern, and the possibility that it might be communicated to a patient, can be avoided if the therapist introduces hypnosis to the patient by discussing naturally occurring hypnotic phenomena and using some of the simple procedures described above to maximize the patient's response. With such an approach to establishing rapport and introducing hypnosis, it is unusual for a patient not to respond to hypnosis, at least to some degree.
Since the time of Breuer and Freud, hypnosis has been widely used in psychotherapy to help patients recall experiences and feelings that they cannot consciously bring up in treatment. The therapist should understand that those memories and feelings may not be historically accurate (that is, they may not have occurred in the ways that the patient describes), but rather they reflect issues that are important to treatment. Although hypnosis can help the therapist to access traumatic material not readily available to consciousness, a therapist should also realize that the patient who does not choose to share an experience rarely will do so in hypnosis.
If a patient is not aware of feelings, however, or cannot readily associate to past experiences, hypnosis frequently provides the opportunity for the patient to recall feelings that may be relevant to a particular issue. In that regard hypnosis can be especially helpful for a patient who discusses events or feelings as if they were happening to someone else. During hypnosis, such a patient can acknowledge having the feelings, so they can be evaluated and dealt with by the patient and therapist, not as though they occurred in the past or to someone else, but as they are felt in the present by the patient.
The literature describes a phenomenon of secondary resistance: a patient initially may have no difficulty entering hypnosis, but later may become unwilling or unable to do so again. As the ability to enter hypnosis is generally a stable attribute, it should be clear that something occurred between the patient and the therapist that bothered the patient. A careful review of what transpired during previous hypnotic sessions should help the therapist recognize and work through the source of difficulty so that the impasse can be resolved.
Perhaps the greatest difference between therapy with a patient not in hypnosis and therapy with a hypnotized patient is that the latter greatly facilitates the development of intense transference feelings. It is not uncommon for a patient, during the first or
1813 HYPNOSIS
second session involving hypnosis, to develop feelings toward the therapist that otherwise may not have developed until much later in treatment -- which can be a problem if it is not anticipated and recognized by the therapist. It is also more difficult for a therapist to observe what is happening in the relationship if the therapist is actively involved in facilitating the patient's experience in hypnosis. For such reasons, a therapist's countertransference feelings are also likely to be more troublesome when hypnosis is used, and may not be as easily recognized as in the traditional, more passive, psychotherapeutic interaction. Consequently, most of the difficulties encountered when hypnosis is used are associated with transference or countertransference issues that have gone unrecognized because of the speed and intensity with which hypnosis brought about the responses. To the extent that they can be recognized and appropriately dealt with by the therapist, they need not interfere with the therapeutic process. Hypnosis does not make such problems different in kind, but only in the speed with which they arise.
If the same issues that bedevil psychotherapy are present when hypnosis is used, then it should be obvious that hypnosis cannot be substituted for knowledge of a particular psychotherapeutic area. For example, a therapist who is not trained in dynamic therapy should not use hypnosis to do dynamic therapy. It is also important to recognize that the same basic therapeutic relationship that characterizes psychotherapy must be maintained when the patient is hypnotized. Thus, a patient's integrity must be respected in hypnosis, just as it is in any ethical psychotherapeutic relationship.
HYPNOANALYSIS
The term "hypnoanalysis" has been used in two ways. It originally described an effort to carry out an extensive therapeutic procedure using hypnosis, but with a process and goals similar to those of psychoanalysis. The approach involves the use of hypnosis to facilitate the availability of dynamic material and the subsequent discussion of that material outside of hypnosis. Typically, a transference neurosis is allowed to develop and is resolved during the later phase of treatment. It is usually considered a more expeditious form of treatment than traditional psychoanalysis, although there is controversy as to whether it achieves the same goals and whether it is more rapid. In this sense, hypnoanalysis has been used by a relatively small number of skilled analysts; it is a very specialized application of hypnosis.
Unfortunately, the term has also been adopted to describe the pseudopsychotherapeutic activity of persons who have limited (if any) psychiatric training, although some of them may be physicians. Often, those practitioners claim to do complete hypnoanalysis over a period of three or four weeks. Their approaches vary, but typically they use hypnosis to encourage intense abreactions, they incorporate a wide variety of suggestions, and they frequently ascribe to pseudopsychobiological theories. They may also treat two or more patients simultaneously using tape recordings that are personalized by the practitioner, who intermittently observes each patient's treatment. Many of them will attempt to regress patients to birth and past lives as part of treatment, and to recover alleged memories as satanic ritual abuse or abductions by aliens from outer space. There is no solid medical or scientific basis for the claims that have been made for hypnotic treatment by such persons.
TREATMENT
DISORDERS OF SELF-CONTROL Many persons view hypnosis as a therapeutic technique to control behavior. For example, when a layperson thinks of hypnosis, it is usually in terms of its potential to treat disorders of self-control, such as to curb smoking, to change eating habits, or to alter cravings for alcohol and other drugs. That impression is reinforced by advertisements of lay hypnotists who purport to treat such problems, often in one or two sessions conducted at a local hotel or auditorium.
In contrast to that widely held view, however, research has failed to document that a person can be induced through the use of hypnosis to carry out behaviors more diligently and more consistently than by other means. Although hypnosis can be employed for those purposes, its effectiveness as a behavior-control technique is limited. In a large series of private patients who sought help to quit smoking, Herbert Spiegel reported that 20 to 25 percent of the patients (as compared with the 85 to 95 percent claimed by lay therapists) responded to a single hypnosis session by remaining abstinent for one year or more.
Many factors affect the likelihood of cessation of a behavior. Persons who seek out a psychiatrist who uses hypnosis are more likely to respond to hypnosis. Similarly, if those persons learned about the therapist through the media, are required to wait for an appointment, or agree to pay a large fee, success is more likely. It is almost impossible to separate those benefits that accrue directly from hypnosis from those that relate to heightened expectation, prestige, suggestion, and the like. From a clinical point of view, it could be argued that it does not matter why a patient responds to a hypnotic procedure, but only that there is a positive response. But if an effect is attributable to hypnosis, there should be a clear correlation between therapeutic outcome and hypnotizability, because the person who is more able to respond to hypnosis should derive more benefit from it. Hypnotizability has been found to have little relationship to long-term smoking cessation. Similarly, most studies of hypnosis in the treatment of obesity have failed to show a correlation between a patient's hypnotizability and success at weight loss. Finally, hypnosis has been unsuccessful in the treatment of alcohol abuse and drug abuse.
Although the hypnotic procedure alone may not be the key factor, it can create the psychotherapeutic context for change in a compulsive behavior, thus exemplifying the use of hypnosis for strategic refocusing.
A 48-year-old executive and father of two teenage sons sought hypnotherapy to help stop smoking cigarettes. During the initial interview, he stated that his company was banning indoor smoking, and, as the senior officer, he realized that he must set an example and enforce the new policy. He stated that he did not want to leave his office building periodically to smoke and requested hypnosis to aid in his smoking cessation. He revealed that he smoked two packs of cigarettes a day, and that he had started to smoke when he was 19 years old, soon after his father, a smoker, had died.
An initial hypnotic trance was induced and recorded on audiotape for his further practice at home between appointments. During the following appointment, he was taught a more rapid induction and several deepening techniques. Negative suggestions regarding the taste and pleasure of his two-decade-old habit were introduced. At the third session, despite conscientious practice, it became apparent that his perception of the desirability of smoking was not changing and he was becoming discouraged. However, he was hypnotically responsive and eager to continue.
In the fourth session he discussed his family life and the desire of his wife and sons to help him feel better physically and to live longer than his father had. Discussion repeatedly centered on his love for his sons and his regret that his own father had not known them. Hypnosis was then induced and it was suggested to him in trance that he began to smoke in memoriam to his father (that is, by smoking as his father did, he would remain forever close to him). To stop smoking would represent a final loss, feelings of which he was unaware, and would require, perhaps, a final act of grieving. Continuing in hypnosis, it was suggested that he could more properly pay tribute to the memory of his father by being a healthier father to his own two sons by quitting smoking. Thus he could continue honoring his father more appropriately rather than compulsively clinging to his past relationship by smoking. He awoke from hypnosis smiling.
1814 PSYCHOTHERAPIES/CHAPTER 31
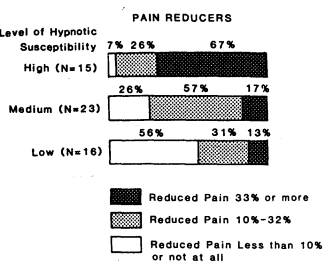
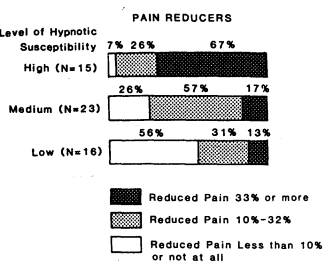
FIGURE 31.3-1 Extent to which subjects with different levels of hypnotizability are able to suppress experimentally induced pain with hypnosis. (Figure from E Hilgard, J Hilgard: Hypnosis in the Relief of Pain. Kaufmann, Los Altos, CA, 1983. Used with permission.)
At the fifth and final session he reported a marked reduction in his smoking and said he felt no desire to continue. On follow-up he had reduced his smoking to several cigarettes at home after dinner. Such an integration of hypnotic techniques in the context of individualized psychodynamic understanding enhances the likelihood of success in treating disorders of self control -- in this case, smoking.
PAIN The suppression of pain by hypnosis, in contrast to disorders of self-control, is highly correlated with the ability of a patient to be hypnotized. Figure 31.3-1 shows the relation as observed in an experimental study of hypnotic pain control.
Although the use of hypnosis for surgical anesthesia is not common because of the availability of effective chemoanesthetics, it has been employed as the sole anesthetic during such surgery as temporal lobectomy, tooth extraction, tonsillectomy, thyroidectomy, pulmonary lobectomy, cardiac surgery, removal of pedunculated folds, bilateral mammaryplasty, appendectomy, cesarean section, hysterectomy, transurethral resection, and excision of varicose veins. The diverse nature of the applications testifies to the fact that at least some patients have the inherent ability to block pain by using hypnosis. Moreover, hypnosis is apparently more than just an emotional tranquilizer, but in responsive persons can affect both the perception of pain and the reaction to pain.
As with other hypnotic phenomena, a patient's ability to be hypnotized and the psychological context in which the hypnosis is used can interact, and so the extent to which either is responsible for pain control is difficult to ascertain. Psychological context can be a powerful factor. For example, in Henry Beecher's studies of the relationship between the significance of a wound and the pain experienced, it was found that soldiers wounded in combat often reported little pain relative to the severity of the wound, required little morphine to control the pain, and were extremely responsive to placebo. In contrast, the pain they felt later, while in a civilian hospital, was more intense and less responsive to active or placebo medication. What differed was the context in which the pain was experienced. In the former being wounded meant escape from the danger of battle; in the latter, the pain represented tangible evidence of illness and was associated with concern over the debilitation that might result from the wound. As a pain-control procedure hypnosis is also subject to such context effects.
Hypnosis is extremely effective as a preanesthetic procedure, often resulting in a decrease in the amount of anesthetic agent needed to achieve the same stage of anesthesia without hypnosis. It is particularly desirable in obstetrics, where its use can decrease or eliminate the need for medications that might affect the baby.
The use of hypnosis to control pain by means of direct suggestions is appropriate and safe when the pain is clearly related to organic lesions or other bodily insult. A wide range of conditions involving acute pain have been alleviated by the use of suggestion, hypnosis, and self-hypnosis. One dramatic illustration was a study by Josephine Hilgard and Samuel LeBaron on the use of hypnosis with children who must undergo periodical bone marrow aspirations for monitoring the treatment of leukemia. Another example of where hypnosis has proved effective in the control of pain of organic etiology, at least for some patients, is in reducing the intense pain produced by the redressing and debridement of burn wounds.
The use of hypnosis with chronic pain, which often involves primarily psychogenic pain, is not generally appropriate. Contrary to what might seem sensible (to use a psychological technique to modify the response to a functional pain), the usual course is initial success followed by sudden ineffectiveness or gradually diminishing effectiveness and the eventual return of pain. The use of direct suggestion for the relief of chronic or psychogenic pain is fraught with difficulties, and it is desirable to combine behavioral therapeutic approaches with hypnosis when treating such pain. The former deal with the secondary gains and other consequences of pain behavior and hypnosis can help a patient to be more comfortable as the functional components of the pain behavior are relinquished.
In some forms of pain that are persistent but may not have significant functional components, such as pain from shingles, trigeminal neuralgia, and many forms of cancer, hypnosis can be a useful adjunct in the long-term supportive treatment of such patients.
An 18-year-old black youth entered a clinical research project that was investigating the use of self-hypnotic techniques to reduce severe, recurrent vaso-occlusive pain resulting from sickle cell disease. He stated that he often missed one to two weeks of school a month because of painful episodes that required narcotics. Sometimes the school absences resulted in hospitalization for intravenous narcotic administration, hydration, and antibiotics; at other times he would stay at home until the pain passed. Despite an average hemoglobin level of 5 to 7 g percent, he maintained a vigorous and relatively normal adolescent life-style.
He was taught self-hypnotic techniques in a group of similar patients ages 6 to 22 years. In weekly sessions over many months he found the techniques easy to learn, but difficult to use on his own when in pain at home, in school, or at the hospital. Each week, with the group, he would discuss his difficulties using hypnosis. Because of his recurring and lifelong pain that would never be cured in the absence of a genetic alteration of his hemoglobinopathy, he was eager to keep trying.
As the months passed, the group members revealed that they had never previously met other patients with sickle cell disease or discussed the problems with them. They acknowledged that medical delivery systems in hospitals and clinics tended to isolate patients and that their many questions had never been shared. Gradually they began to confront each other with their concerns: How long would they live? Would they require cholecystectomy and hip replacements? How likely were the chances of stroke, fatal pneumonia, and complications of teenage pregnancy and childbirth? As questions and answers began to alleviate their isolation and fears, realistic expectations became more commonplace and anxiety was reduced.
The young man started to use self-hypnotic techniques at home and, with practice, was able to alleviate minor and moderate sickle cell pain Confidence in his ability to cope and manage his future with fever narcotics and with less absenteeism allowed him to obtain an apprenticeship as a carpenter after high school graduation. He is now living in his own apartment and uses self-hypnotic techniques with continued success.
The joint use of self-hypnosis and group psychotherapy allowed the best of each treatment modality to combine to influence and change his life experience.
1815 HYPNOSIS
ANXIETY DISORDERS Anxiety disorders are among the conditions that are most frequently treated with hypnosis or meted techniques. There is some evidence that as a group persons with phobias tend to be more readily hypnotizable than the population at large. Fred Frankel has proposed that the development of phobic anxiety is related to spontaneously occurring hvpnoticlike states. Thus, the trance experience may provide a coping mechanism. For example, a patient may recognize the similarity between a frightening depersonalization experience and the feelings associated with the patient's first hypnosis by a therapist. The latter, however, was under the patient's control in a supportive psychotherapeutic context, which permitted the patient to cope with what had previously been anxiety-provoking feelings.
The relaxation and feelings of comfort that accompany the induction of hypnosis have often been effective in allowing a patient to gain control over phobic symptoms or generalized anxiety. Self-hypnosis can provide a tool that permits the patient to relax and thereby control or eliminate the response to a stimulus that aroused fear outside of the therapeutic context. It is easy to conceive of the relaxing effect that hypnosis or self-hypnosis can produce as a physiological response that is incompatible with anxiety or fear. In the Wolpe reciprocal inhibition technique used in the behavioral treatment of phobia, a patient learns to master fear by being able to relax, thereby becoming able to tolerate stimuli that had previously produced intense fear.
A 30-year-old opera student requested hypnosis to overcome her stage fright during auditions. She stated that she was talented and known for her stage presence during amateur and school performances. She insisted that medication, such as propranolol (Inderal), be avoided because she felt it might dampen her onstage creativity.
After the initial evaluation, self-hypnotic techniques were introduced and an audiotape recording was made of the session for practice at home. Emphasis was placed on deep breathing consistent with the operatic breathing techniques in which she already was skilled. During a subsequent session she readily progressed to creating a quiet, safe place where no anxiety existed. By using the image and peaceful feelings of that place, she could imagine increasingly anxious scenes from her auditions without fear. By systematically desensitizing her fears, she was able to relax more during actual performances. In hypnosis emphasis was then placed on allowing her more freedom for innovation on stage.
Long-term success depended not only on traditional systematic desensitization, but on also utilizing hypnosis to enhance the patient's creativity.
Hypnosis has been used in the psychodynamic treatment of anxiety to help a patient recall material associated with the etiology of the phobia. In that approach hypnosis is integrated into the overall psychodynamic strategy. Self-hypnosis can be used to help control episodes of anxiety. Similarly, hypnosis and self-hypnosis can be important adjuncts to the treatment of the intense fear and anxiety associated with the posttraumatic stress disorder.
PSYCHOLOGICAL FACTORS AFFECTING MEDICAL CONDITION Perhaps the most interesting applications of hypnosis involve the use of suggestion to treat conditions that appear to have a physiological etiology. When hypnosis is effective in such instances, there is often no way to understand the mechanism by which the healing is effected or why other patients fail to benefit from hypnosis. Systematic studies to clarify whether hypnotizability is a key factor in the cure of medical disorders have yet to be carried out, and the defining of brain mechanisms by which hypnosis may provide relief is speculative.
Some carefully conducted clinical studies are available, however, in which patients were randomly assigned to hypnotic or standard medical therapy. A British study of hypnotic control of asthma attacks found that hypnosis was significantly more effective than the standard medical treatment. Similarly, an extensive study of migraine headache sufferers, with patients randomly assigned to hypnosis or ergotamine tartrate (Ergomer) treatment, found that hypnosis was significantly more effective in controlling migraine attacks. Neither of those studies assessed hypnotizability, however, so it is not clear what roles the hypnotic condition, the hypnotic relationship between patient and physician, and patient expectancies played in the improved treatment outcomes.
Single-case studies in which hypnosis dramatically improved medical conditions have also been reported. For example, a case of congenital ichthyosis that was documented by skin biopsies was successfully treated with hypnotic suggestion by a young physician who mistook the symptoms for warts. The condition was present bilaterally on the patient's body. The therapist used hypnosis to suggest that the right hand would develop normal skin. When the right hand cleared, the therapist used hypnotic suggestion to clear the left hand. Histology demonstrated that sebaceous glands were present in the skin after hypnosis whereas previously there had been an atresia. The fact that there are no other reports of congenital ichthyosis resolving with any treatment makes the case report unique, although there have been many unsuccessful attempts to treat cases of ichthyosis by means of hypnosis.
The treatment of warts by suggestion has been a time-honored part of folk medicine. One type of wart (verucae planae juvenilia) has been shown to respond to hypnotic suggestion in several studies, but other studies have failed to confirm its effectiveness. There is too much evidence in the literature to dismiss the effectiveness of hypnosis and suggestion in treating warts, but there is no compelling explanation of how a psychological intervention can affect resistance to a viral infection.
A 19-year-old unmarried woman was referred for a spasm of accommodation requiring + 14 diopters of correction. The patient was barely able to see with correction and required a drop of atropine in each eye to provide temporary normal vision (a drop of atropine typically blurs vision for hours). Among the many medical procedures conducted on the patient was a craniotomy to expose the optic chiasma, which did not reveal any pathology. As a last resort the patient was referred for hypnosis treatment in the hope that she might either obtain relief or learn to cope with the problem. During psychotherapy it became clear that she had ambivalent feelings toward her father and a male friend. During hypnosis, the patient reported that the first accommodative spasm had occurred during a ski trip when she did not want to see what transpired between her male friend and another woman. In a stormy session about two years into therapy she suddenly maintained that her spasm was self-induced and that she had used the symptom to cope. Her vision improved markedly; she was able to see with modest correction and within two months her vision was normal. She continued to insist that the problem had been self-induced and that she could produce the spasm at will. On subsequent examination by an ophthalmologist she voluntarily produced a spasm of +7 diopters, but she could not go beyond that to the + 14 diopters with which she had originally presented. Follow-up over several years showed that she continued to function with normal vision. Psychotherapy and hypnosis appeared to be instrumental in helping the patient to overcome what was assumed to be a medical problem, but the precise manner in which it took place is unclear.
Another illustration of the use of hypnosis as an adjunct to the treatment of a medical condition thought to have an organic etiology is that of a patient with intractable hiccups following surgery.
A 56-year-old man had undergone chest surgery and shortly thereafter developed intractable hiccups presumed to be related to a phrenic nerve disorder. The hiccups had continued without remission for two days and the patient was becoming progressively more debilitated because he was unable to rest and sleep. A psychiatric consultation was requested in the hope that the hiccups could be stopped. After establishing rapport with the patient, it was necessary only to induce a profound level of relaxation and then suggest to the patient that he would be able to continue to sleep comfortably. The frequency of hiccups diminished markedly during the prolonged induction procedure, and stopped as the patient appeared to go to sleep. The patient was awakened that evening to be given his sleeping medication, whereupon he again began
1816 PSYCHOTHERAPIES / CHAPTER 31
to hiccup. The episode was readily controlled with the same slow induction procedure, whereupon he slept through the remainder of the night without interruption. The hiccups did not recur until late the next day. The patient was again relaxed and instructed in how to hypnotize himself in order to become comfortable. He was followed over several days and was able to control the very minor residual symptom without additional help. Hypnosis and self-hypnosis appeared to be effective in controlling a debilitating physical symptom.
There are many other instances in which treatment involving hypnosis has helped medical conditions, although it is difficult to understand the mechanisms that facilitated healing. Even the basic question of the importance of the patient's ability to enter hypnosis in effecting improvement remains unanswered; for example, a patient with psoriasis may show dramatic remission after hypnosis, whereas another patient may fail to improve despite experiencing profound hypnosis. In one by David Spiegel study in which hypnosis was used in a psychosocial group treatment context, a retrospective analysis revealed that patients afflicted with metastatic breast cancer lived longer than did those in the control group. Such examples suggest a far greater role for psychological factors in the exacerbation and remission of physical symptoms than might be assumed. Understanding the mechanisms by which hypnosis improves some physical symptoms should ultimately shed light on the manner in which feelings, thoughts, and fantasies affect physical health.
DISSOCIATIVE DISORDERS
Dissociative amnesia and dissociative fugue Hypnosis has long been used to help patients overcome the memory loss of amnesia and fugue. Even persons who suffer from the most extreme dissociative memory deficits continue to have access to their general fund of knowledge; they typically score about the same on intelligence tests as they did before the fugue or amnestic episode. Similarly, there is no loss of language ability nor are there problems in knowing what constitutes appropriate behavior in their subculture. A patient does not lose memory storage but the ability to access it in terms of past experiences. For example, a patient experiencing fugue may be able to describe a graduation ceremony, but may not be able to describe his or her own graduation. Thus a patient will be unable to remember what has happened and yet continue to have social and intellectual skills.
One approach to the treatment of fugue and dissociative amnesia is to induce hypnosis and to suggest that a patient will recollect events that have happened. Although the results of such an approach may be impressive to an observer, a direct suggestion to lift the amnesia is often undesirable because dissociative fugues and amnesias occur for dynamic reasons, and are the kind of symptoms that should be dealt with cautiously to avoid the possibility of even more inappropriate expressions of the underlying problem. Rather than attempting to eliminate the amnesia, it is generally best to use hypnosis to explore the events that precipitated the fugue or amnesia. Those events can be discussed with a patient during trance at considerable length. Before the patient comes out of hypnosis, however, it is important to make clear that the patient may choose to forget some, or even all, of what was remembered during hypnosis (until the patient has worked out alternative ways to deal with the problems). Not only is that approach safer than suggesting away the amnesia, but it also provides the therapist with important information in terms of what the patient does or does not recollect after the session. The aim of the treatment should be to help the patient cope with the underlying problem and not to attempt to force the patient to relinquish the symptom until able to do so comfortably.
Dissociative identity disorder Like dissociative fugue states, dissociative identity disorder (formerly multiple personality disorder) traditionally has been considered a rare disorder. There has been a close association between dissociative identity disorder and hypnosis from the time the disorder was first identified before the turn of the 20th century. In many of the original cases the alter personality states were elicited by a therapist while the patient was in hypnosis. Moreover, persons who suffer from the disorder have consistently been described as highly hypnotizable.
A key part of the diagnostic criteria of dissociative identity disorder, according to the fourth edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), is the presence in a person of two or more distinct personality states that recurrently take control of behavior. There is an inability to recall personal information, and the disturbance is not attributable to substance abuse or a general medical condition. It appears that the basic problem in dissociative identity disorder is a distortion of memory or an amnesia. The memory store containing the general fund of knowledge is not split among the different personality states, but is shared by them. Clinical research has shown that if a secondary personality state is given words to remember, a memory savings on these words is observed in the recollections of the primary personality, although there is no conscious awareness by the primary personality of the words that were learned. In dissociative identity disorder some personality states may be aware of others; typically, an alter personality state is aware of the original personality, but the original personality is unaware of the alter personality state. Additional personalities may be aware of some but not of others.
Examples of the memory problems that accompany dissociative identity disorder include patient complaints of being unable to recall what was done at certain times, reports of finding their belongings in strange places or finding strange items among their belongings, and reports of comments on behavior of theirs that was uncharacteristic and of which they have no recollection. Typically, the diagnosis is confirmed by the therapist's eliciting one or more preexisting personality states during hypnosis. Those personality states are often able to account for the lost time, blackouts, and the memory problems of the primary personality state.
Morton Prince, around the turn of the century, reported a celebrated case of multiple personality disorder that prompted the first of many acrimonious disputes about the reality of the disorder. Criticism ranged from claims that such patients were faking the condition to the view that the therapist produced the disorder through the use of hypnosis. Controversy over the nature and etiology of dissociative identity disorder continues to the present. Up until the early 1970s very few patients with multiple personality disorder were identified, and most of the cases, such as that of "Eve" by Corbett Thigpen and Hervey Cleckley, were presented in the professional literature. Until the past two decades, the condition was viewed as extremely rare. That view has changed dramatically in recent years. For example, more diagnoses were made of the condition in 1990 alone than in the 75-year period from 1895 to 1970.
Although psychiatric diagnoses wax and wane in popularity, the current trend toward diagnosing dissociative disorders appears in part to have its origin in the manner in which psychotherapy in general, and the use of hypnosis and suggestive therapeutics in particular, are currently misapplied by some practitioners in the diagnosis and treatment of dissociative disorders. If that is the case, then the spontaneous dissociative identity disorder may still be rare, and its increased prevalence in recent years may be understood in terms of contagion and iatrogenic and socioeconomic factors.
DIAGNOSIS To understand dissociative identity disorder, it is important to recognize that no one displays a truly consistent personality. Significant others are introjected into a person's personality, and different contexts bring out aspects of personality that may not be consistent with other aspects. The appearance of consistency is created by the fact that a person will recall carrying out many (but not all) of those quite inconsistent behaviors, and so acknowledge each as his or her own by rationalizing them to make them congruent. Given a person's tendency to dissociate and forget actions that he or she would not like to recall, it is not strange for someone to say, "I could not have done that. I don't recall it."
A presumptive diagnosis of dissociative identity disorder may impel a therapist to explore the possibility that the patient's behavior can be understood as reflecting the existence of a new, previously unknown personality state. The typical way in which an alternate identity is evoked is by a therapist's asking to speak to a different part of the patient. That technique is most frequently utilized during hypnosis, but the same request can be effective without formal hypnotic induction. If the patient accepts the invitation and displays what appears to be an alternate identity, there is no guarantee that what follows reflects a true dissociated personality state, but is an ego fragment that the patient wishes to make known to the therapist. If the therapist then asks the patient, "What is your name?" and a different name is given, which the therapist accepts and thereby legitimizes, the basis for an alternate identity has been created where one may not have existed or at least did not fully exist previously
As with the behaviors of hypnosis, the manifestations of various kinds of pathology, such as dissociative identity disorder, are affected by the culture and the beliefs of the persons with whom the patient comes into contact. A therapist's expectations will profoundly affect treatment outcome. Considering that hypnosis greatly enhances transference and countertransference, and that therapists are generally dealing with highly hypnotizable persons when dissociative symptoms present, it is not surprising that the incidence, severity, and number of dissociative identity disorder cases have risen dramatically since the second and third editions of DSM (DSM-II and DSM-III) helped to legitimize the diagnosis in the psychiatric community.
Traditional dynamic psychotherapy is characteristically committed to helping patients take responsibility for their behaviors and to understand the feelings that cause those behaviors. Once a therapist begins
1817 HYPNOSIS
to accept an alternate identity as essentially a different person, the respnsibility for the patient’s behavior and feelings is relegated to that alternate identity. That relegation is particularly pronounced if the therapist implicitly endorses the dissociative identity disorder by accepting secrets that are to be kept from one or the other personality state. It becomes even more difficult as the therapist feels obliged to treat each of the alternate identities as a patient, while recognizing the need to help the various components ultimately to come together. The situation can become exceedingly complex as the therapist becomes aligned with some parts of the patient and against other parts.
The etiology of dissociative identity disorder is generally believed to be related to abuse and trauma during childhood, and it is common to inquire about such abuse during hypnotic age regression. Some therapists are successful in eliciting such reports whereas others are not. Certainly, the manner in which the inquiry is made has much to do with the likelihood of obtaining reports of physical, sexual, or mental abuse.
In considering how dissociative identity disorder should be diagnosed, it must be kept in mind that the expectations of a therapist regarding the incidence of the disorder are likely to influence the frequency with which the therapist diagnoses it. It will also have an effect on the number of personality states a patient demonstrates. For example, the number of personalities in a given patient seen by Prince and his contemporaries was typically three or four, whereas today it is commonplace to hear of more than 10, or even more than 100, alternate identities in a patient. And although Prince rarely found suicidal or destructive personalities, such alternate identities are the rule in today's dissociative identity disorder cases. The extent to which alternate identities are destructive and suicidal will vary in terms of both the patient's and the therapist's expectations, as well as the percentage of patients who are profoundly depressed or borderline and acquire the diagnosis of dissociative identity disorder.
TREATMENT The use of hypnosis is often advocated in the treatment of dissociative identity disorder. The procedure usually involves calling forth the various personality states, gradually making each identity aware of the others, choosing various techniques to facilitate communication among them, and ultimately fusing the identities in ways that allow the prosocial and ego-syntonic personality states to control and encompass the destructive components of the negative personality states. It is hoped that the ultimate fused personality can draw strength from the previously disparate identities.
In an alternative approach to the treatment of dissociative identity disorder the therapist accepts the reality that the patient has a variety of conflicting feelings, as well as difficulties with memory. The therapist avoids asking an ego fragment for its name and it is not treated as a different identity or personality state. Rather, the therapist takes the position that everyone can be inconsistent and that there are memories, feelings, and actions that can be in conflict and that need to be understood. Regardless of how repugnant those experiences and feelings might be, and regardless of the difficulty in remembering them, they are still the patient's feelings and actions. Most important, the therapist avoids falling into the trap of becoming the confidant or accomplice of one part of the patient vis-à-vis another part, and does not reify the existence of the alternate identities and run the risk of becoming a coopted party to whatever intrapersonal conflict is involved. By not becoming a participant in the intrapsychic conflict and by refusing to accept that there is more than one identity, albeit one with many inconsistent feelings, the therapist is able to help the patient assume responsibility for various thoughts, feelings, and actions. The patient may have trouble in becoming aware of past actions and memories, but as awareness develops, those feelings can be understood and integrated as a part of the self, regardless of how alien they may have been perceived initially.
Hypnosis may still be used very effectively, but care should be taken neither to force a patient to remember something that is unacceptable nor to help hide something that a person is unwilling to discuss. A technique that can be helpful if used judiciously is to record the sessions and allow a patient to listen to the tapes in order to become aware of the events that occurred during treatment. If a patient is afraid to listen to a given session, the therapist should be willing to listen to the tape with the patient. Occasionally, a particularly crucial session will require more than one opportunity to review it in the therapist's presence. Those procedures are important because the patient’s problem is one of memory; without the dissociative capacity a person cannot develop an identity disorder. The use of tapes in treatment does not prevent the patient from discussing material that is important and difficult, but it does provide a way for the patient to become aware of feelings and actions that had previously been kept from consciousness.
It would be incorrect to argue that the clinical syndrome of dissociative identity disorder does not exist. However, owing to the bizarre nature of the disorder and its description in an increasing number of books and films it would be surprising if a number of some patients did not come to believe that they were suffering from dissociative identity disorder and develop alternate identities, just as a person may come to believe that he or she is possessed after viewing a film or hearing a sermon about possession. If the belief is intense enough, it may lead to serious dissociative phenomena. The role of hypnosis in the treatment of such dissociative disorders ought to be to facilitate integration of the person rather than to provide an opportunity for the reification of alternate identities.
In her second year of psychotherapy for depression, paranoid delusions, and problems resulting from a difficult marriage, a 50-year-old woman stated that she had eight personalities. She had responded to antipsychotic and antidepressant medication in the past and had made several constructive adjustments in her relationship with her husband.
During a regular appointment she brought in a written list of her personalities with their characteristics and needs for therapeutic attention. She did not have large gaps in her memory and felt she was aware of each personality. She maintained that she had a high-grade multiple personality disorder. She asked whether hypnosis might not be helpful in giving her main personality more time to express her own interests as a person rather than, as she stated, waste time while the other various personalities dwelled on her problems with other people in her past and present. She denied childhood physical or sexual abuse, but acknowledged emotionally damaging relationships during her years of growth and development.
Further discussion over the next several sessions revealed her belief that she had always had a tendency to dissociate. She explained in metaphor that, as several slide projectors can fade and replace an image seamlessly on one screen, she had been able to shift imperceptibly from one personality to another all her life. However, when maximal stress occurred, she said, she would dissociate more discretely. She described those experiences as similar to many slide projectors abruptly showing separate images on the screen, causing her confusion and anxiety. The nature of those major stresses related to current issues with her husband, her children, and her desire to start a responsible job outside the home for the first time.
Her request for hypnosis was declined, as further insight into the nature and the role of her personalities could easily be achieved outside of hypnosis. Integration of her personalities would be enhanced by confronting and reducing the various stresses in her life, not by manipulating, in hypnosis, the boundaries separating her various ego states. It was agreed that with further growth and self-assertion, she might become further integrated, similar to eight slide projectors simultaneously showing her various personalities on the same screen and gently fusing them into one person. She agreed that she could work on maintaining the best (and perhaps even the worst) of each personality in creating the complexity of one normal human being.
CONTRAINDICATION
Although hypnosis is generally safe when used by a competent clinician, there is a basic guideline that should always govern its use. A therapist should never attempt to use hypnosis with a patient or in the treatment of a condition that the therapist is unable or unwilling to treat without hypnosis. If that guideline is not followed, the clinician will be acting out the fantasy that hypnosis makes it possible to treat conditions that are beyond his or her expertise.
The induction of hypnosis with a healthy person is innocuous, particularly when the person does not expect any permanent changes to result from the experience (for example, in an experimental situation). However, when hypnosis is induced in clinical contexts, it acquires the same problems that are seen in psychotherapy in general. The typical complications that arise in therapy involve transference and countertransference issues, which are greatly enhanced in the use of hypnosis. It is crucial for the therapist to remain aware that the same dynamic factors that pertain to a dyadic therapeutic relationship also apply when hypnosis is used in therapy, although the therapist's activity may make it more difficult to recognize nascent difficulties before they begin.
The problems that are seen when the therapist's rescue fantasies are not recognized are particularly prone to occur when hypnosis is used because of the quasi-magical fantasies easily evoked in both the patient and the therapist. As with any adjunctive technique, hypnosis can be misapplied or used in a manner that exacerbates an overall poor treatment strategy. Because it plays on the power fantasies of patients and therapists, it is important that hypnosis never be utilized in a coercive manner.
1818 PSYCHOTHERAPIES/CHAPTER 31
Establishing rapport with a patient before the induction of hypnosis is essential to avoid power struggles and to maximize the likelihood of a productive therapeutic experience. Because hypnosis can accelerate and amplify the therapeutic interaction, its use requires that the therapist maintain all the skills required in psychotherapy. Under no circumstances should it be assumed that a patient is so deeply hypnotized as to be unable to appreciate the significance of the therapist's words or actions. For example, it is never appropriate to discuss a patient with a colleague while the patient is hypnotized. All the rules of courtesy and respect for patients apply when hypnosis is used in treatment.
It remains controversial as to what extent highly hypnotizable persons can be coerced into doing things or saying things that are contrary to their values and beliefs. Nevertheless, the therapist is responsible for ensuring that the suggestions given in hypnosis are ethical and not contrary to the patient's moral code. The suspension of critical judgment by the hypnotized patient, together with the heightening of transference and countertransference through hypnosis, also make it imperative for the therapist to examine the treatment goals carefully lest the hypnotic procedure become a vehicle for exploiting the patient's vulnerabilities. If a therapist has difficulty in maintaining an objective and respectful stance toward a patient, hypnosis will make the situation worse.
Hypnosis can be used as an adjunct to the treatment of a wide array of disorders, but it is not generally appropriate for psychotic disorders. For example, few therapists have used hypnosis to treat schizophrenia or severe depressive disorder. There is controversy about the extent to which persons with schizophrenia can be hypnotized. On the Stanford Scales of Hypnotic Susceptibility the distribution of scores of patients with schizophrenia is similar to that of healthy persons, except that such patients forget (in response to an amnesia suggestion) far more items than normals, and fail to recall those items when the amnesia is lifted. If the hypnotic assessment involves complex cognitive demands, such as is the case with the Spiegel Hypnotic Induction Profile, then persons with schizophrenia score significantly lower than normals. It is fair to say that, except in the hands of a few therapists, hypnosis has no significant role in the treatment of schizophrenia.
It is also best to avoid the use of hypnosis with paranoid patients because such patients can easily integrate hypnosis into their paranoid systems. Delusions of having been hypnotized are common among patients with paranoia even when they have never been hypnotized, and the therapist may be unable to treat a paranoid patient following a hypnotic induction.
Severe depression is not relieved by hypnosis because patients who suffer from it generally do not respond to hypnotic induction when they are severely depressed. Manic patients are equally difficult to hypnotize, and there is little advantage in attempting to do so.
HYPNOSIS AND MEMORY
AGE REGRESSION Hypnosis continues to be widely used to aid in the recall of significant material in the therapeutic context. It is typically used to facilitate memories of important events, particularly events involving intense emotions. In hypnotic age regression the patient's speech, movements, and posture, as well as the quality of the interaction, suggest to an observer that the person has become a child again. As the patient relives the traumatic event intense affect characteristically is displayed, which is so realistic that it is difficult to imagine that anyone could act that well. The description of the event includes observations that presumably could not have been made unless the patient had actually been there -- facial expressions, the light coming through the window, the picture on the wall, and so on. Finally, when hypnosis is terminated, the patient will often experience relief of the symptom that was associated with the past event.
The vividness of such experiences originally convinced Freud that age regression truly induced a return to earlier life events and his early theories on hysteria were directly related to those observations. He soon realized, however, that the apparent memories from the hypnotic relivings were not veridical, although they were psychologically important and useful.
The therapeutic technique of age regression is still used, and has continued to convince some clinical observers that the patient is reliving the past, reexperiencing what it was to be a child, and recalling actual childhood events. Drawings by age-regressed hypnotized subjects appear to be childlike and seem to be convincing proof of the reality of the hypnotic age regression. Systematic studies have been carried out, comparing the drawings of hypnotically age-regressed subjects with the drawings of children of that age. Experts in child drawings described them as sophisticated oversimplifications, and had no difficulty in discriminating them from actual drawings by children. Figure 31.3-2 compares the age-regressed drawings of a subject with drawings the person had made as a child and had not seen since. Although the age-regressed drawings (B, C) look childlike, when compared with the actual drawings made by the subject as a child (A), they are seen to be totally different.
Research has failed to substantiate the belief that accurate memories are reinstated by hypnotic age regression. From a therapeutic point of view, it should be emphasized that historical truth is not what bothers a patient -- it is what the patient originally perceived, or thinks was perceived, and what has remained as part of the patient's memories over the years. Although that mixture of memorial fact, inference, interpretation, and confabulation may only slightly resemble what actually occurred, it is more important in the patient's psychopathology and eventual recovery than are the historical facts. Donald Spence speaks of that distinction when differentiating the narrative truth that is obtained in psychotherapy from the often poorly correlated historical truth of the matter.
One aspect of the memories brought out during hypnotic age regression, which has long been a reason why they were felt to have been accurate, was that they often resulted in unsuggested symptomatic improvement. It is worth noting that Janet had already demonstrated in the late 19th century that helping patients to remember the past with hypnosis, and then changing the memories to be more ego-syntonic (for example, suggesting that a patient won in a game with an older brother rather than having lost) had positive therapeutic consequences. In the 1940s Milton Erickson used similar techniques successfully. Therapeutic improvement cannot be used to validate the accuracy of recollection. Clearly, hypnotic age regression can be a powerful therapeutic tool regardless of the accuracy of the memories or the belief in them by the therapist, as long as the patient and therapist work through the feelings represented in the memory reports. It is prudent to follow Freud's example and not encourage the patient to act on hypnotic age-regression memories outside of the therapeutic setting.
MEMORY ENHANCEMENT The use of hypnosis for memory enhancement outside of the therapeutic context has been widely touted as a reliable and valid means of assessing the recollections of witnesses to crimes and victims of crimes. Although an overwhelming body of research indicates that hypnosis does not increase accurate memory, it does increase the
1819 HYPNOSIS
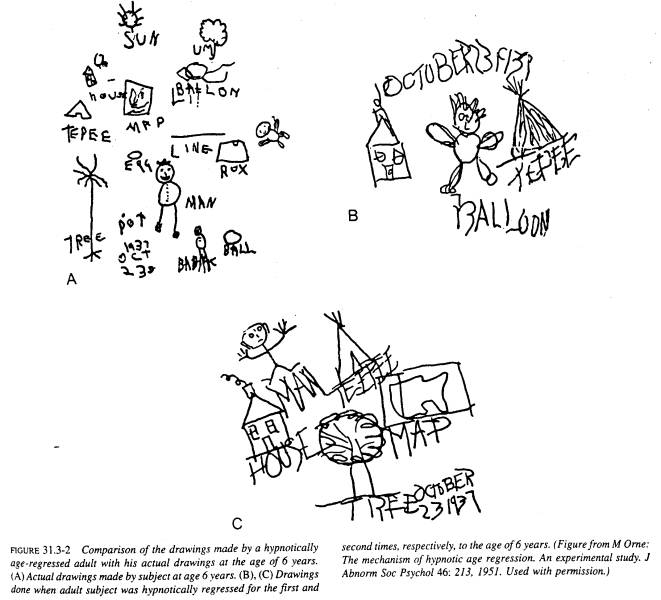
person's willingness to report previously uncertain memories with strong conviction. Furthermore, the hypnotized person has a pronounced tendency to confabulate in those areas where there is little or no recollection; to distort memory to become more congruent with beliefs, hopes, and fantasies; and to incorporate cues from leading questions as factual memories. There is also the likelihood that the beliefs of the hypnotist will somehow be communicated to the patient in hypnosis and incorporated into what the patient believes to be memories, often with very strong conviction.
Hypnosis has been accepted as a therapeutic modality by the American Medical Association (AMA), the American Psychiatric Association, the American Psychological Association, and the British Medical Association, as well as by many other professional groups. None of those organizations nor the relevant scientific research community has endorsed the use of hypnosis to aid the recall of witnesses to crimes or victims of crimes, and the AMA adopted, in December 1984, a formal position cautioning against its use in that capacity. The AMA also points out that hypnosis is not a way of assuring truthful reports, as a person is capable of lying, even under deep hypnosis, as well as of faking hypnosis. Those caveats should be kept in mind lest an attempt be made to use hypnosis or amobarbital (Amytal) to validate the accuracy of statements made by patients. The use of such techniques will only serve to confuse the physician, the patient, and the public, and will not assure reliable answers. Hypnosis is simply not a reliable means of enhancing memory or of obtaining historical truth.
Given the risks of factually inaccurate information, care should be taken not to use hypnosis or other techniques involving suggestions in attempting to elicit statements concerning sexual abuse. Although there is a widely held view that false-positive detections of sexual abuse are preferable to allowing a single case to remain undetected, the nature of hypnosis is such that a false-positive outcome is far more likely when it is used. The consequences of a child's losing the support of one or both parents as a result of such a false-positive detection must be considered when a therapist encourages a patient to believe in events recalled in hypnosis.
Hypnosis can facilitate fantasy, creativity, and the ability to control physiological and psychological mechanisms in a manner conducive to physical and mental health. The ability to recall psychologically meaningful events is important, and the fact that they need not be accurate could be a major reason why
1820 PSYCHOTHERAPIES/CHAPTER 31
hypnosis can accelerate dynamic therapy by allowing a patient to rectify some aspects of the past and to make it more acceptable, in order to facilitate going forward rather than ruminating about the past. However, those attributes of hypnosis also make it exceedingly dangerous as a means of eliciting testimony where establishment of fact is the primary objective. Hypnosis is a powerful therapeutic tool, but like any catalyst it needs to be employed at the right time; interpretation of the results of its use must take into account the nature of the catalytic action and the context in which it occurs.
CONFABULATION AND CHILD ABUSE Disorders of memory are most painful when one's identity and recall of personal history are affected. Without the awareness of either patient or therapist, historical truth becomes blurred and narrative truth may be accepted as factual, especially when supported by strong feelings. Memories of events recovered in hypnosis, or with hypnoticlike techniques can be perceived uncritically as actually having happened. Recently there has been a return to the misconception that childhood trauma -- in particular, childhood sexual abuse -- underlies many psychiatric problems, and that health is achieved when patients accept as factual newly recovered memories of traumatic events.
Unlike psychodynamic insights regarding the motivation for certain behaviors, the assumptions of those who embrace the historically accurate-childhood-trauma theory of memory are that the past events are evidenced by even the most subtle nuances of behavior, and that the memories of them are encapsulated like videotapes in the brain or body, awaiting discovery in psychotherapy and hypnosis. Once recovered, the patient's gaps in memory are filled, confidence in the newly recovered confabulations is gained, and with those decade-delayed memories the patient becomes an eyewitness, ready to confront those persons now believed to have perpetrated the original trauma. Therapists create enormous problems when they understand memory and hypnotherapy in such terms, especially when they take feelings, or believed-in newly discovered happenings, outside the therapeutic setting to confront the family or effect retribution in the legal process.
It is critical to remember that child abuse does occur and is sometimes reported many years later. However, hypnosis is not a truth serum, and when used as such, hypnosis and related techniques of suggestion can transform the therapeutic setting into a stage for the iatrogenic induction of increased dependence on fantasy and confabulation. The misunderstanding of hypnosis as a kind of truth serum that accesses a neural "videotape" of recorded memories (for which there is no scientific support) is at the basis of the increasing acceptance of false memories and serious consequences they entail for the patient and the family.
Certainty about repressed memories brought forth under hypnosis or hypnoticlike techniques is a direct result of the suggestions of the therapist and the trust that patients place in the therapeutic setting. Thus, if a patient reports headaches and other somatic symptoms and is told by a therapist that the cause can be found in past traumas to be uncovered by hypnosis or hypnoticlike techniques, the stage is set for confabulation, and the result will likely be a patient who becomes confident that childhood sexual abuse or satanic ritual abuse actually took place. Indeed, that expectation can be established in some receptive and trusting patients even by a mere waking suggestion, convincingly administered by a therapist or hospital staff member that a particular physical or psychological symptom probably reflects traumatic abuse in childhood. Unfortunately, by indiscriminately interpreting virtually all physical and psychological symptoms as indicative of childhood abuse, confabulated memories of such events by patients can harm both the patients and their families
A 30-year-old salesman and his parents sought an independent consultation for family therapy. The man related the following: He had previously entered psychotherapy for vague feelings of unrest, depression, and listlessness. After a physical examination was negative, he had sought counseling. Slowly during the course of his therapy, he began to focus on the difficult family interactions that had colored his youth. Having been afforded some relief by antidepressant medication, he wanted to continue his searching his past for "the reason" for his current life difficulties.
In the belief that current life experiences often reflect those of earlier years, he asked his therapist to hypnotize him to facilitate his search for earlier memories. One day, in trance, he imagined that his mother, on tucking him in bed when he was a child, had kissed him longingly and lovingly. He became very frightened of the memory.
In subsequent sessions he and his therapist explored the meaning of the memory and gradually, without any corroborating evidence but with the therapist's acceptance, the patient concluded that he had been sexually abused as a child by his mother. A confrontation between the patient and his parents ensued. His parents denied the accusation, and the patient then severed communication with them.
In contrast to many such cases, the patient and his parents eventually sought an independent consultation to resolve the stalled communication. During a single session, each family member overcame intense feelings and began to talk. There was no corroborating evidence of abuse, although the family acknowledged that the mother, throughout her son's adolescence, had bought her son's clothing, including his pajamas. The patient had described that practice as further proof that his mother must have sexually abused him.
The patient, now comfortable that he was fully respected by both the consultant and his parents, began to smile at his distortion of his mother's routine purchases in support of his possible memory recovered in hypnosis. Whether false or not, the memory was soon seen to be less important than his current and future problems of separation and independent growth. Although many issues remained for further therapy in highly dysfunctional family, the consultation restarted their dialog in constructive ways.
Guidelines exist for using hypnosis in evaluating patients with suspicions of having been abused as children, which may make future therapy for such families less painful and more effective.
Most psychiatrists and psychologists accept the need to develop therapeutic alliance, gain insight into the lifelong antecedents of the chief complaint, and work through hard-won insights to relieve suffering and effect change as a critical task. However, increasing numbers of therapists favor the seemingly easier method of rapidly eliciting hypnotic "memories" of abuse in childhood. Vivid memory reports, abreaction, and the idea that hypnosis (like amobarbital) is a truth serum further enhances the certainty experienced by the therapist and the subject. Armed with those insights patients and therapists release their anger and conceptualize recovery as retribution. The unfortunate result is that patients learn to blame others rather than to accept personal responsibility for their own actions. Hypnosis can be effectively used to help a patient strategically refocus away from searching for past "memories," and turn instead toward effective assertiveness in personal and professional endeavors.
A 54-year-old married female school teacher sought hypnotherapy to recover possible memories of childhood sexual abuse. She stated that during normal loving sexual relations with her husband, she sometimes would "drift off" and find it difficult to be fully attentive. Her family life was otherwise normal. She noted that, during her administrative duties, she often found it difficult to express her opinions assertively despite the high regard in which her colleagues held her and her abilities.
In the first session the controversies regarding the veridicality of recovered memories by hypnosis was discussed. She stated she wanted to use those memories, if they existed, as material for psychotherapy, and not as material for a legal suit or recrimination outside the therapist's office. She supported the request by stating that the suspected perpetrator was dead.
Hypnosis was induced easily. She rapidly learned the principles of self-hypnosis and deepening techniques. Age regression occurred smoothly in trance over a number of sessions, and various images of abuse appeared during the ages of 6 to 9 years. Each image differed in detail, and some contradicted others. Nonetheless, corroborating evidence was suggested by various family photographs and reports by siblings that the patient collected for therapy. In any event, the patient
1821 HYPNOSIS
and the therapist agreed that something may have happened. Gradually, after the hypnotic exploration was completed, anger and rage emerged, which seemed to the patient to be related to the childhood abuse. Many other events in her life, unrelated to the abuse, also surfaced during her nontrance psychotherpay that added to her anger and fear. One by one they were examined, and a pattern of unexpressed rage and aggression soon emerged. It became clear that by repressing her anger and rage throughout her life, she had also lost access to other deep emotions, such as love, joy, and excitement.
As she progressed in her understanding that her emotional life was restricted by fear of her rage, she took responsibility for learning to be more assertive and aggressive in her personal and professional life. Whether the memories of her abuse were accurate, the process of her psychotherapy was enhanced by her discovering an acceptable reason anger and an understandable cause for its repression. The goal of her therapy was not retribution, even if the alleged perpetrator had been alive, but to permit the patient to live more fully in the present. She succeeded. When the goal is revenge and blame, personal growth seldom ensues.
Increasingly, accusations of abuse confront families seeking help for their sons and daughters for a wide variety of traditional psychiatric syndromes, including depression, difficult personal relationships, eating disorders, generalized anxiety states, and paranoid delusional syndromes. The use of hypnosis or hypnotic techniques can never justify a therapist's substituting confabulation, accusations, and confrontation for doing the work of therapy and encouraging patients to accept responsibility for their own motivations and behaviors.
SUGGESTED CROSS-REFERENCES
The biology of memory is discussed in Section 3.5 and psychoanalysis in Section 6.1 and 31.1. Anxiety disorders are the subject of Chapter 17 and dissociative disorders are presented in Chapter 20. Chapter 26 discusses psychological factors affecting medical condition. Evaluation of psychotherapy is discussed in Section 31.10.
REFERENCES
Baker R A: Hidden Memories. Prometheus Books. New York, 1992.
Bliss E: Multiple Personality, Allied Disorders and Hypnosis. Oxford University Press, New York, 1986.
Bloom P B: Clinical guidelines in using hypnosis in uncovering memories of sexual abuse: A master class commentary. Int J Clin Exp Hyp 42: 3, 173, 1994.
Brown D, Fromm E: Hypnosis and Behavioral Medicine. Erlbaum, Hillsdale, NJ, 1987.
*Crasilneck H, Hall J: Clinical Hypnosis: Principles and Applications, ed 2. Grume & Stratton, Orlando, 1985.
Dinges D, Whitehouse W, Orne E, Powell J, Orne M: Evaluating hypnotic memory enhancement (hypermnesia and reminiscence) using multitrial forced recall. J Exp Psychol 18: 5, 1139, 1992.
Ellenberger H: The Discovery of the Unconscious: The History and Evolution of Dynamic Psychiatry. Basic Books, New York, 1970.
*Frankel F: Hypnotizability and Dissociation. Am J Psychiatry 147, 823, 1990.
Frankel F, Perry C, editors: Hypnosis and delayed recall: Part I [special issue]. lnt J Clin Exp Hyp 42: 4, 1994.
Frankel F, Perry C, editors: Hypnosis and delayed recall: Part 11 [special issue]. Int J Clin Exp Hyp 43: 2, 1995.
Fromm E, Kahn S: Self-hypnosis: The Chicago Paradigm. Guilford, New York, 1990.
Fromm E, Nash M: Contemporary Hypnosis Research. Guilford, New York, 1992.
Ganaway G: Historical versus narrative truth: Clarifying the role of exogenous trauma in the etiology of MPD and its variants. Dissociation 2: 205, 1989.
Hilgard E, Hilgard J: Hypnosis in the Relief of Pain. Kaufmann, Los Altos, CA, 1983.
*Laurence J-R, Perry C: Hypnosis, Will, and Memory: A Psycho-Legal History. Guilford, New York, 1988.
Lynn S, Nash M: Truth in memory: Ramifications for psychotherapy and hypnotherapy. Am J Clin Hyp 36: 3, 194, 1994.
Ome M: The mechanisms of hypnotic age regression: An experimental study. J Abnorm Soc Psychol 46: 213, 1951.
*Ome M. Bates B: Reflections on multiple personality disorder: A view from the looking glass of hypnosis past. In Mosaic of Contemporary Psychiatry in Perspective, C Pierce, M Greenblatt, A Kales, editors. Springer-Verlag, New York, 1992.
Ome M, Bauer-Manley N: Disorders of self: Myths, metaphors, and the demand characteristics of treatment. In The Self. Interdisciplinary Approaches, J Strauss, G R Goethals, editors, p 93. Springer-Verlag, New York, 1991.
*Ome M, Dinges D: Hypnosis. In Textbook of Pain, P Wall, R Melzack, editors, p 1021. Churchill Livingstone, New York, 1989.
Orne M, Wender P: Anticipatory socialization for psychotherapy: Methods and rationale. Am J Psychiatry 124: 9, 1968.
Orne M, Whitehouse W, Dinges D, Ome E: Reconstructing memory through hypnosis: Forensic and clinical implications. In Hypnosis and Memory, H Pettinati, editor, p 21. Guilford, New York, 1988.
Pettinati H: Hypnosis and Memory. Guilford, New York, 1988.
Rhue J, Lynn S, Kirsch I: Handbook of Clinical. Hypnosis. American Psychological Association, Washington, 1988.
Spence D: Narrative Truth and Historical Truth: Meaning and Interpretation of Psychoanalysis. Norton, New York, 1982.
Spiegel D: Living Beyond Limits. Times Books, New York, 1993.
Spiegel D, Bloom J, Kraemer H, Gottheil E: Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet 2: 888, 1989.
Whitehouse W, Orne E, Ome M, Dinges D: Distinguishing the source of memories reported during prior waking and hypnotic recall attempts. Appl Cogn Psychol 5: 51, 1991.
Figure 31.3-1 (p. 1814) (from Hilgard, E.R., & Hilgard, J.R. Hypnosis in the relief of pain. Los Altos, CA: Kaufmann, 1983.) is reproduced here with the kind permission of William Kaufmann.
Figure 31.3-2 (p. 1819) (from Orne, M.T. The mechanism
of hypnotic age regression; An experimental study. Journal of Abnormal and Social
Psychology, 1951, 46, 213-225.)is reproduced here with the kind permission of
the American Psychological Association © 1951. No further reproduction
or distribution of this figure is permitted without written permission of the
publisher.