How is Vitamin D Formed?
Vitamin D is a prohormone. This means that it does not act as a hormone
itself; instead, it must be converted within the body to a molecule
that does have hormone activity (20).
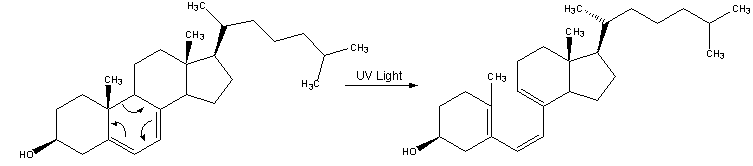
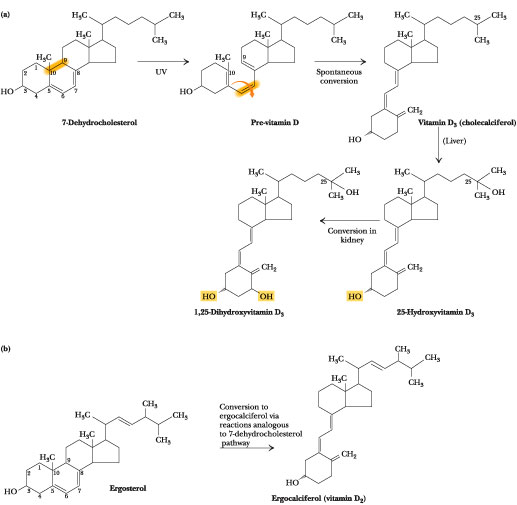
Vitamin D3 is made in the skin when the skin is exposed to
sunlight. Specifically, the UVB light from the sun reacts with
7-dehydrocholesterol to produce the cholecalciferol. The UV light
wavelengths must be in the range of 270 to 290 nm if they are to be
effective at converting the 7-dehydrocholesterol to vitamin D3 (20).
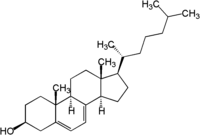
7-dehydrocholesterol (
http://en.wikipedia.org/wiki/7-Dehydrocholesterol )
http://i115srv.vu-wien.ac.at/uv/COST726/COST726_Dateien/WG3/graphics/AS_VitaminD_McLaughlin.gif
Additionally, vitamin D3 will only be made in adequate amounts after 10
to 15 minutes of sun exposure at least twice a week. The skin
needs to be directly exposed to the sunlight, without the presence of
sunscreen or clothing. If in the sun for an extended period of
time, once an adequate supply is generated, any additional vitamin D3
degrades so that an equilibrium is achieved (3, 14, 20).
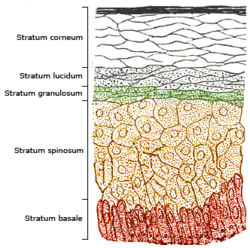
The skin consists of two layers: the dermis, which is the inner
layer of the skin, and the epidermis, or the outer layer of the
skin. The epidermis can be further stratified into the stratum
corneum, stratum lucidum, stratum granulosum, stratum spinosum, and
stratum basale. (These are listed from the outermost layer to the
innermost layer) (3, 20).
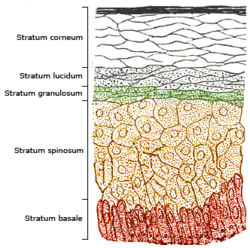
Layers of the Skin (http://en.wikipedia.org/wiki/Vitamin_D)
7-dehydrocholesterol is located in highest concentration in the
epidermis, specifically within the stratum basale and stratum
spinosum. Therefore, production of vitamin D3 will be greatest in
these layers because this is where the main concentration of its
precursor is located. Other layers of the skin will produce
lesser amounts of vitamin D3 because the have lesser concentration of
the 7-dehydrocholesterol.
UVB light only effectly penetrates the epidermal layers of the
skin (3, 20).
UV Light
The sun emits various types of radiation, including ultraviolet (UV)
radiation. This radiation has very short wavelengths and very
high energy. UV radiation can be further categorized into UVA
(400-320 nm), UVB (320-280 nm), and UVC (less than 280 nm).
Although all of these types of radiation are released from the sun,
Earth's atmosphere absorbs a majority of it. Therefore,
approximately 99% of the UV radiation that actually reaches Earth's
surface is UVA. The rest of the radiation that reaches the
surface is UVB (the UVC is stopped in the ozone layer) (22). This
small amount of UVB is enough to allow for the production of vitamin D
within the skin. This UVB is absorbed by the
7-dyhydrocholesterol, and the molecule is converted to cholecalciferol
through photolysis and subsequent isomerization (3, 4, 14, 20).
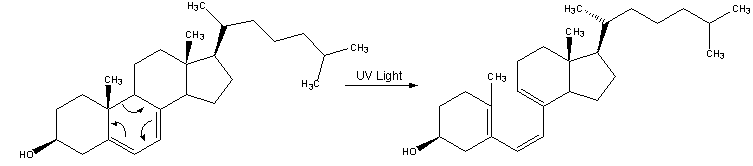
Transformation of 7-dehydrocholesterol Upon Absorbing Ultraviolet Light
(
http://www.search.com/reference/Vitamin_D)
To the Liver
At this point, the vitamin D3 is still inactive. It moves to the
liver via the blood. Specifically, it is carried by carrier
proteins. When it reaches the liver, it undergoes
hydroxylation by an enzyme called 25-hydroxylase. The vitamin D3
is now converted to 25-hydroxycholecalciferol, also known as
25(OH)D3. It is stored until it is needed. The half-life of
this compound is several weeks, so it lasts for quite some time before
it degrades (3, 14, 20).
Off to the Kidneys
Here, the 25(OH)D3 is hydroxylated yet again by the enzyme
1-alpha-hydroxylase, creating 1,25-dehydroxycholecalciferol, or
1,25(OH)2D3. This is the biologically active form of vitamin
D. The synthesis of this active form is more tightly controlled
than the production of any of the precursors. The half-life of
this form is only a few hours (3, 14, 20).
And Finally to the Rest of the Body
At this point, the active form is released again into the circulatory
system. Here it binds to another carrier protein called the
vitamin D binding protein (VDBP) and is transported to other
organs. When it gets there, the vitamin D binds to a vitamin D
receptor (VDR). The VDR also has a site available for binding to
DNA. When the complex binds to the DNA, it acts as a
transcription factor in that it modulates transcription, in some cases
activating transcription, and in others, suppressing it.
Transcription is the process of producing RNA and ultimately
producing peptides. The VDR typicallyl modulates the proteins
which ultimately are involved in the absorption of calcium in the
intestine. However, the vitamin D receptors are located in most
organs, not just the intestine. The VDRs play different roles
accoring to their location (20).
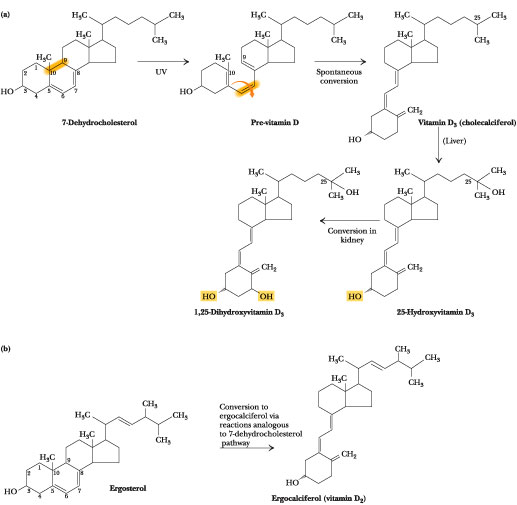
The Entire Metabolic Process of Vitamin D Formation
(
http://www.web.virginia.edu/heidi/chapter18/chp18.htm)